ALF MAGNE HORNELAND
Building a system of evidence-based medical selection, requires a structured approach to the assessment of fitness for work and risk related to reduced function or acute failure due to a medical incident whilst in service on board.
In the following, we will discuss the step-wise risk assessment recommended in the Guidance[1] to the Norwegian regulations on medical examinations of employees on Norwegian ships and mobile offshore units.
C.8.8.1 First step: The identification of possible medical incidents
Given a known medical condition in a seafarer, the medical examiner will be able to identify which possible medical incidents that could occur as a complication, a relapse, a deterioration or an episode in connection to the underlying medical condition.
Medical condition | Possible short term medical incidents | Possible long term medical complications |
Insulin-dependent diabetes mellitus | Episode of hypoglycaemia Episode of hyperglycaemia | Retinopathy Nephropathy Neuropathy Myocardial ischemia Stroke Intermittent claudication |
Table 3: Example of possible incidents related to underlying medical condition – diabetes mellitus | ||
Whilst the long-term medical complications are important to the future job prospects, they are not so important in medical selection for a period of two years ahead. The short-term incidents, however, are of utmost importance to the assessment.
The maximum validity period of a medical certificate according to the international conventions[2] [3] and guidelines[4] today, is two years. Then a new assessment is required. Whether or not the seafarer will be able to work for many years is not important to the decision regarding his working ability during the next two years. It is, however, expected that the medical examiner informs the seafarer about the importance of lifestyle and proper treatment of the condition, to be able to preserve his fitness for work for many years, not only for the nearest two year period.
Similar to the above example, an approved doctor can identify possible medical incidents in most cases where he knows the medical condition. Sometimes the condition can be of more unclear nature, like a loss of, or reduced concentration or ability to prioritize, problems with keeping up focus, being aware and staying awake, possibility of being irritable, suffering from anxiety or getting depressed. In such cases, the model of risk assessment connected to incidents is not so suitable. In such cases, assessment of working capacity is more interesting.
C.8.8.2 Second step: The ‘general’ likelihood of medical incidents
Not many published scientific articles focus on the likelihood of a medical incident occurring in the next two years, at least not the types of incidents we need to assess in medical selection. They seem to focus on so-called ‘hard end-points’, which means that many possible incidents are not included in the studies. Such studies consider relapse, re-intervention, survival and death usually in a period of 1, 5, and 10 years.
Sometimes we can find data that apply to the group of individuals to which the seafarer belongs, other times we cannot. We often have to use a heuristic, probabilistic approach, where the medical examiner has to follow his best judgement based on sound practice.
In assessing this ‘general likelihood’, systematic review studies rank above single studies, for obvious reasons. Some very good review databases exists, like the UpToDate[5], BMJ Best Practice[6] and Cochrane[7].
Sometimes we find the likelihood for a short-term outcome, given a specific condition and its stage or level of seriousness. It often requires long periods of reading and searching, longer than can be expected that medical examiners can use for searching in their daily work. Those who develop regulations, standards, criteria and guidelines should preferably provide such data and make them available to the medical examiners. The Norwegian Guidance to the health regulations[8] is an attempt to do this.
C.8.8.3 Third step: The ‘individual likelihood’ of medical incidents
For several good reasons, one should be careful not to put too much emphasis on a consideration of the ‘general likelihood’ as found from studies.
Reviewed articles are often published years after the study has been finished and researchers know the result. New practices often are implemented before the study is published.
Individuals have very different prognoses, depending on many factors. Consequently, there is a need for individualisation, a process that could be carried out starting from an understanding of the ‘general likelihood’.
In other parts of clinical medicine, biomarkers are useful in attempts towards individualization of prognosis[9] [10]. Most doctors are familiar with assessment of prognosis based on staging of different types of cancer using the TNM system[11]. It is, however, not very likely that such helpful tools will be available for the purpose of medical selection.
The below table visualises how factors related to the individual and severity of condition will influence how the approved doctor assesses the likelihood of a medical incident in a two year period.
Individual factors | Medical condition factors | Environmental factors |
|
|
|
Table 4: Prognostic factors in medical selection. | ||
It is not possible to carry out a statistical calculation of how likely it is that an individual will get a medical incident within two years. This makes it difficult to carry out risk assessment during a PEME. Even though, the medical examiner has an obligation to make up his or her mind regarding how likely it is that the incident with a potential of harm could occur. This is the ‘noble art of medical selection’.
Specialist advice
In the process of estimating the individual likelihood for a medical incident, advice from a relevant medical specialist can be valuable. However, the specialist usually is not well informed about the health requirements, either statutory or employer/insurer specific. The specialist should be asked to give an estimate of the likelihood in a two-year perspective, based on his updated knowledge of the professional field and knowledge about the individual’s medical condition and records.
To avoid misunderstandings, the specialist should be informed about the relevant health requirements and job demands, as well as the definition of likelihood.
The specialist on likelihood is the treating specialist. The ‘specialist’ on risk assessment is the approved doctor.
C.8.8.4 Fourth step: The consequences, when a medical incident occurs
Looking at the Figure 2, the cascade reaction after a medical incident, a number of different consequences could be expected. A number of factors have influence of the severity of the consequences, as listed in the table below (Table 5). It is obvious that a reliable risk assessment cannot be carried out unless the seafarer’s profession, position, job tasks, ship type, trade area and crew size are taken into account.
This means that the medical practitioner cannot perform the required assessment without knowledge about shipboard life, and the specific knowledge about the seafarer and his position. It is of utmost importance that this is included in the training of seafarers’ doctors.
Factors related to the working place | Comments | |
Department | Deck | Navigation and manoeuvring tasks, risk of collision, grounding, shipwreck |
Engine | Maintenance and emergency responses | |
Catering | Risk of contagious diseases and food poisoning | |
Situation | Ordinary activities | Regular duties may not be carried out |
Emergency situation | Critical duties may not be carried out Capability of being a firefighter with breathing device? | |
Trade area | Near Coastal | Easier to follow up a medical incident in port |
High seas | Outside reach of MEDEVAC possibilities | |
Time at sea | Long time for necessary follow-up | |
Distance from SAR service | More serious consequences in emergency cases | |
Littoral waters | Grounding in minutes or seconds if manoeuvring errors | |
Redundancy | Spare hands available | Being the only engineer leaves the ship without that capacity if he falls ill. Will someone take over? |
Type of ship | Tanker | Risk of safety consequences to ship, crew and environment, financial losses |
Cruise ship | Risk for passengers, delays, reputation of company, insurance | |
Table 5: Factors of importance to consequence assessment. | ||
This also emphasizes that carrying out a risk assessment, solely with the specification of ship department, without linking this to the position on board a specific ship in a specific trade, makes little sense.
It is unfortunate that the job position is not required on the recommended certificate form under the STCW and MLC 2006 Conventions[12] [13], and that it is not an obligation to get a new medical when changing position, ship, trade, and trade area. This needs to be included in the future, as it is obvious that the consequences may be very different with the same position in the same department in different trade areas and on different ships.
Example 1, below, describes two scenarios with the same profession, same job position, but different trade area and ship, with few consequences on one occasion and a disaster on the other occasion.
It is of utmost importance that medical examiners have an understanding of shipboard life. Personal experiences are valuable, but will often be limited to one type of ship. The basic training of medical examiners should ensure that doctors get the necessary insight regarding working places and job tasks on board ships.
Example 1: A mate on the bridge, during a night watch, on a cargo ship in transatlantic trade, still one week from shore, going on autopilot systems, suddenly becomes incapacitated. This probably will have little consequences for ship and crew, and the consequences to him/her-self will be limited to those of the medical incident and the distance to shore and possibilities for MEDEVAC. A mate on the bridge, during a night watch, on a fast passenger ship in littoral waters, like along the Norwegian coast, manoeuvring manually in addition to being responsible for the navigation, suddenly becomes incapacitated. This could imply running on shore with 100 passengers on board in a few seconds, with disastrous consequences for the passengers, and loss of many lives. CONCLUSION: The same profession, the same medical condition, the same position on board – tremendous differences in consequences, hence also risk, when the same incident occurs. |
C.8.8.5 Fifth step: Estimation of the un-mitigated risk
Risks can be mitigated in different ways, but remedies used for mitigation, like hearing aids, glasses, contact lenses and medicines, can be delayed or even lost during a flight, forgotten at home, lost by accidents or theft. The result will be that the seafarer exposes the ship, crew and self to the unmitigated risks of the medical condition.
Having a well-controlled hypertension, then losing the medicines, could result in acute complications from an uncontrolled blood pressure. Being dependent on contact lenses, getting a bilateral conjunctivitis and having forgotten to bring spare glasses, leads to a complete different situation than what would have been the case if the seafarer had glasses available. The examples of similar situations are numerous.
The importance of always considering un-mitigated risk, not only the mitigated risk, should be clear. Even if the condition usually will be mitigated and well controlled, there is always a chance that tablets could be thrown up because of sea sickness or a gastrointestinal condition, have less effect because of diarrhoea, are lost, stolen, delayed, cannot be replenished etc.
The ‘formula’ mentioned in Figure 2, shows how ‘risk’ could be estimated.
RISK (POTENTIAL LOSS) = LIKELIHOOD (FOR INCIDENT) X CONSEQUENCES (WHEN INCIDENT OCCURS).
In principle, such a risk assessment could lead to three different results:
- Acceptable
- Acceptable if mitigated
- Not acceptable
The matrix in Table 6, which serves a pedagogic purpose, illustrates this assessment:
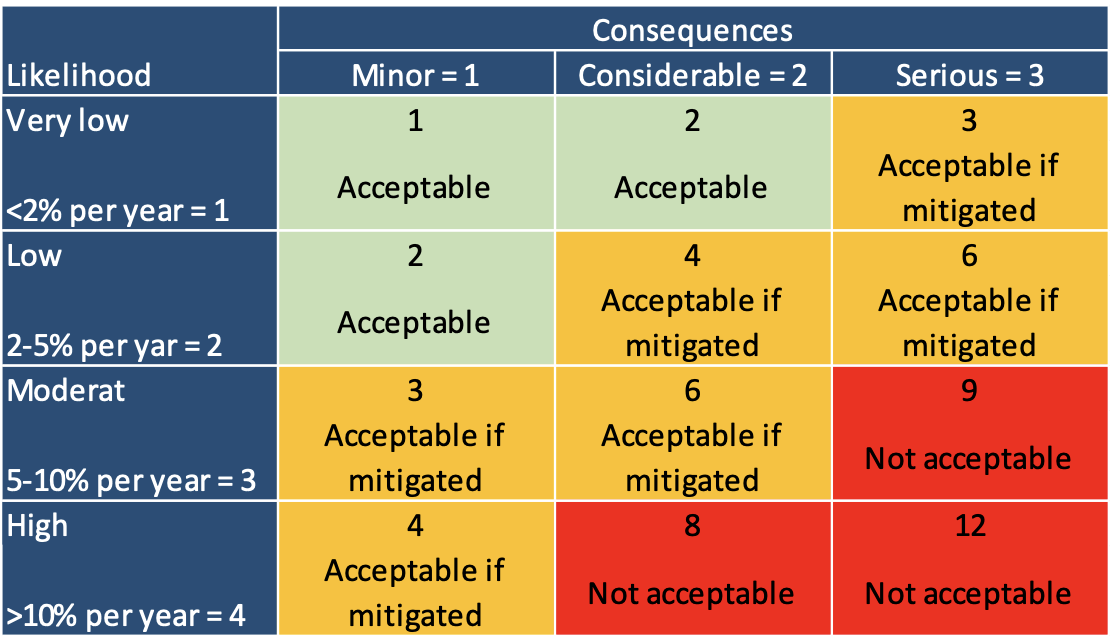
Table 6. Matrix for the assessment of unmitigated risk.
The left column lists likelihood in four rows, corresponding to the definition of the verbal terms found in the Norwegian regulations, with reference to the ILO/IMO guidelines. One definition of the different levels of likelihood should be agreed and used commonly. We recommend the definition found in the Norwegian regulations. Agreement on definitions is prerequisite for more reliable and reproducible estimates by different medical examiners.
The upper row lists three different levels of consequences: minor, considerable and serious. Theoretically, the matrix could include more columns on consequences, but the three we have chosen, serve the purpose of illustration. In principle, we can get three different estimates: ‘acceptable’, ‘’acceptable if mitigated and ‘not acceptable’.
The matrix emphasizes the fact that a very low likelihood, combined with minor consequences, leads to an acceptable risk. On the other hand, a high likelihood and serious consequences, should lead to the estimate of an unacceptable risk.
In between the two conclusions there will be a grey zone (or amber zone), where the risk could be acceptable if it is sufficiently mitigated, but unacceptable if not mitigated.
There are many cases where a risk is acceptable, provided proper mitigating measures are in place, whilst at the same time is unacceptable, should those mitigating measures not be available.
The assessment of un-mitigated risk serves the purpose of providing an understanding what would be the consequences, should the symptoms of the condition be present in full bloom, as would be the case in situations where medicines are lost, stolen, delayed during a flight or not possible to replenish. Examples could be individuals with hypertension, diabetes, Addison’s disease not getting their usual treatment, or glasses, lenses and hearing aid that are lost.
The medical examiner has to consider the different types of risk in accordance with the purpose of the regulations, guidelines, statutory programme or enhanced PEME scheme. How large is the risk to the seafarer him/her-self, to the safety of the crew and ship, to the operation, to a big financial loss?
4.8.1.6 Sixth step: Risk mitigation
Possible mitigating measures vary with the condition. They fall in different categories, as shown in Table 7 below.
Types of mitigating measures | ||
Type of mitigating measures | Mitigating measure | Example |
Measures that reduce likelihood of a medical incident | Medicines | A large number of medical conditions treated with medicines |
Reduced validity period | Where short-term prognosis is fairly good, but more uncertain in a longer perspective | |
Close follow-up by a specialist/hospital or approved doctor | To ensure that changes in condition/prognosis is detected before they result in a ‘medical incident’ | |
Measures that reduce the impact of a dysfunction | Glasses or contact lenses* | Myopia, hypermetropia, astigmatism, presbyopia |
Hearing aids | Hearing loss | |
Alarms | ||
Measures that reduce the consequences of a medical incident | Near coastal traffic | Quicker access to medical assistance and hospitalisation |
Restriction in position on board | Not sailing as captain No solo watchkeeping No part of the bridge watch No safety function | |
Measures that increase preparedness | Information to ship’s master regarding condition and use of medicines | |
Preparedness medicines | Injectable steroids for cases of Addison’s crisis | |
Measures that correct a bodily dysfunction | Refractory surgery | For myopia |
Prosthesis | Limb amputation | |
Surgical intervention | Gall stones, urinary stones | |
Table 7: Examples of mitigating measures * In cases where the seafarer usually wears lenses, glasses should always be a backup. They could be used also in cases of superficial eye infections or minor eye trauma, where lenses cannot be used. | ||
The measures that corrects a bodily dysfunction requires a separate comment.
Refractive eye surgery as a mitigating measure
Even if the incidence of complications are low, some of the surgical methods used for correcting distance vision, have complications that give reason to consider their use in this context. McDonald et al.[14] documented the risks of getting night vision difficulties and glare. They also demonstrated that under- and overcorrections occur, resulting in need for LASIK retreatment in 10.7% of patients. Regression to preoperative vision sometimes occurs with time[15]. There is a 0 to 3.6% loss of two or more lines of best spectacle corrected visual acuity reported with laser refractive surgery[16] [17] [18] [19]. Rare cases of corneal perforations are reported[20]. Dry eyes are common following laser refractive surgery[21]. Astigmatism, including irregular astigmatism can occur[22] [23]. Glare, halos and monocular diplopia can occur postoperatively[24]. Night halo can also remain a problem for many years[25]. Newer generation excimer laser has oblation profiles to minimize the transition of treated and non-treated cornea in an attempt to reduce these symptoms. Some postoperative patients develop a loss of contrast sensitivity following laser refractive surgery[26], which in some cases could be incompatible with standing a bridge watch or function as a lookout.
Cholecystectomy in cases with asymptomatic gallstones
Some of the enhanced PEME schemes require that asymptomatic gallstones found on an ultrasound screen must be removed before going to sea. It is important to notice that prophylactic cholecystectomy is not indicated for most patients with asymptomatic gallstones since the risk of developing life-threatening, severe complications is low, and if symptoms do occur, they are generally mild initially. Prophylactic cholecystectomy slightly decreases survival and is not associated with an appreciable gain in discounted life-years gained[27]. The model was constructed prior to the development of laparoscopic cholecystectomy, but it is unlikely that the laparoscopic approach would significantly alter the results based upon the results of the sensitivity analysis included in the study[28]. There is good reason to be cautious in recommending cholecystectomy in asymptomatic individuals.
Hearing aids
The use of hearing aids could improve hearing loss. However, pure tone audiometry does not assess understanding of speech, and is not suitable for testing the level of hearing in people using hearing aids. Speech audiometry would be a better way to assess hearing in such cases. We lack, however, criteria for such assessment. In the end, this is a political decision – which risk is acceptable, and which risk is unacceptable. Studies in the working environment on board are missing. To mirror the real life communication, speech audiometry preferably should be carried out with background noise, such as engine and wind noise and noise from people talking.
C.8.8.6 Seventh step: Estimation of the mitigated risk
Under ordinary circumstances, the mitigated risk is the relevant one. The unmitigated risk relates to exceptional situations (like in emergencies), which often have a very low likelihood of occurrence, but still have to be included.
In considering the mitigated risk, once again one have to look at different aspects, like risk to self, risk to crew, ship or operation, or – if it should be a part of the requirement – risk of financial loss.
The medical examiner should answer the following questions before deciding on conditional certification:
- Which conditions/mitigating measures should apply to the medical certificate – if any?
- How much will the mitigating measures reduce the likelihood?
- How much will this reduce the severity of the consequences?
- How well is a dysfunction compensated?
- Is the overall risk acceptable when the necessary conditions are set?
- Will it require consideration by a superior body to set the conditions for service, or could the approved doctor set the conditions?
- How realistic is it for the seafarer to be able to work on board on a conditional basis?
- Are the conditions having a disproportionate negative impact on the person or persons subject to the differential treatment?
- Are the conditions of decisive significance for the performance of the work or the pursuit of the occupation?
When the approved doctor scrupulously have considered these questions, he should be able to compare his own, stand-alone assessment with the requirements of the PEME scheme he is following. That is the next step.
C.8.8.7 Eight step: Comparison with the statutory requirements
As mentioned earlier, the PEME schemes represent a heuristic approach to finding those who are fit for service at sea and excluding those who are unfit. However, the criteria of the standards are only to a small extent based on evidence. In addition, as they are not revised continuously whilst the development of diagnostic and treatment possibilities in medicine is accelerating, it is to be expected that the AD sometimes will find that his assessment is not concurrent with the criteria of the scheme.
Three different results of this comparison is possible:
Alternative 1: The AD finds that his assessment is equal to the requirement of the criterion
Alternative 2: The AD finds that his assessment points to a more lenient decision than the criterion requires
Alternative 3: The AD finds that his assessment points to a stricter decision than the criterion requires
Alternative 1 is the easiest one. Then the AD issues a certificate in concordance with the criterion, and he will be able to justify this decision towards the seafarer not only by pointing to the statutory basis and criterion. He will also be able to explain to the seafarer why this is the right conclusion, based on a risk assessment and medical information.
Alternative II is a situation where the AD finds that the criterion is too strict, and cannot be justified (see Ch. 4.8.3). Despite this, he cannot issue a certificate incongruent with the requirements, but he has a very good reason to support the seafarer to apply for an exemption or dispensation, and is able to justify why this is defensible and reasonable. He also has a good basis for approaching the relevant authority or party that has issued the regulations, about this case, for use in future revisions of the regulations.
Alternative III is trickier. What to do when the requirements obviously are too lenient for the case? First, the AD should double check that he finds the seafarer noncompliant with the purpose and the objectives of the regulations or guidelines. If this is so, he should issue a certificate of unfitness, and explain that the seafarer has the right to appeal his decision. In the appeals process (see below), he is well prepared to explain why he thinks this decision is right, despite what the guidelines says. At the same time, this offer an opportunity for the appeal instance to consider whether the regulations should be revised, and initiate the proper process.
Ninth step: Conclusion and justification of the assessment
After the questions above have been scrupulously considered, the AD should be able to decide, and substantiate his decision in a way that can serve as information to parties concerned with the work, like the seafarer, an appeal instance, an employer, an insurer, or whoever could be entitled to such explanation.
For seafarers’ doctors approved by the Norwegian Maritime Authority, the requirements of the Norwegian Public Administration Act apply. Among other obligations, there is an obligation to substantiate the decision and inform the seafarer, in writing, regarding the conclusion.
If the AD has followed this model of risk assessment, he should be able to explain, not only the legal requirements and criteria, but the medical background for why this is the correct decision.
By a first glimpse, the model may look complicated, but in most cases is not time-consuming for the trained user. It has some advantages.
- It makes the AD able to justify and defend his conclusion
- It makes it easy to prepare a case for the appeals instance
- It makes it possible to assess the existing criteria against up-to-date knowledge
- It improves the skills of the AD, who will build his personal competence in assessment of seafarers
- It makes it possible for the professional environment to better understand the nature of the medical selection process, increase the awareness and hopefully and eventually, build the evidence that is lacking today.
References
[1] Guidance to regulations on the medical examination of employees on Norwegian ships and mobile offshore units, ver 2.3. – Norwegian Maritime Authority, 8th June 2018, https://www.sdir.no/contentassets/4d82128b4fd649e9921993d2073fc2f0/veiledning-til-helseforskriften.pdf?t=1557821105933
[2] MLC, 2006, Standard A1.2, Paragraph 7.
[3] STCW Convention, 1978, Regulation A-I/9.
[4] Guidelines on the medical examination of seafarers, Ch. VI Purpose and contents of the medical certificate, Paragraph 2.
[5] www.uptodate.com from Wolters Kluwer
[6] https://bestpractice.bmj.com/
[8] Guidance to regulations on the medical examination of employees on Norwegian ships and mobile offshore units, ver 2.3. Norwegian Maritime Authority, 8th June 2018. Freely accessible at the www.sdir.no
[9] Draikiwicz S, Oppenheimer J. Patient Characteristics and Individualization of Biologic Therapy. Immunol Allergy Clin North Am. 2017 May;37(2):261-281. doi: 10.1016/j.iac.2017.01.004. Epub 2017 Mar 1. PMID: 28366476
[10] Donskov F, Heng DY, Rini BI. On-treatment biomarkers in metastatic renal cell carcinoma: Towards individualization of prognosis? Expert Rev Anticancer Ther. 2017 Feb;17(2):97-99. doi: 10.1080/14737140.2017.1269605. Epub 2016 Dec 20. PMID: 27927054.
[11] TNM Classification of Malignant Tumors (TNM), developed by the Union for International Cancer Control (UICC), 1968, later amended many times, and merged with the staging system used by the American Joint Committee on Cancer (AJCC) in 1987.
[12] ILO/IMO Guidelines on the medical examination of seafarers, Sectoral Activities Programme ILO/IMO/JMS/2011/12. Appendix F. Suggested format for recording medical examinations of seafarers.
[13] ILO/IMO Guidelines on the medical examination of seafarers, Sectoral Activities Programme ILO/IMO/JMS/2011/12. Appendix G. Medical certificate for service at sea.
[14] McDonald MB et al. Laser in situ keratomileusis for myopia up to -11 diopters with up to -5 diopters of astigmatism with the summit autonomous LADARVision edcimer laser system. Ophtalmology. 2001;108(2):309.
[15] Chayet AS et al. Regression and its mechanismes after laser in situ keratomileusis in moderat and high myopia. Ophtalmology. 1998;105(7):1194.
[16] McDonald MB et al. Laser in situ keratomileusis for myopia up to -11 diopters with up to -5 diopters of astigmatism with the summit autonomous LADARVision edcimer laser system. Ophtalmology. 2001;108(2):309.
[17] Hersh PS et al. Photorefractive keratectomy versus laser in situ keratomileusis for moderate to high myopia. A randomized prospective study. Ophtalmology 1998;105:1512.
[18] Kawesh GM, Kezirian GM. Laser in situ keratomileusis for high myopia with the VISX laser. Ophtalmology 2000;107:653
[19] Watson SL, Bunce C, Allan BD. Improved safety in contemoporary LASIK. Ophtalmology 2005;112:1375
[20] Hori Y et al. Medical treatment of operative corneal perforation caused by laser in situ keratomileusis. Arch. Ophtalmol. 1999;117(10);1422
[21] Battat L et al. Effects of laser in situ keratomileusis on tear production, clearance and the ocular surface. Ophtalmology. 2001;108(7):1230
[22] Krueger RR et al. Clinical analysis of steep central islands after excimer laser photorefractive keratectomy. Arch Ophtalmol. 1996:114(4):377.
[23] TamaYO Fernandez GE, Serrano MG. Early clinical experience using custom excimer laser ablations to treat irregular astigmatism. J Cataract Refract Surg. 200:26(10):1442
[24] Hersh PS, Steiner RF, Brint SF. Photorefractive keratectomy versus laser in situ keratomileus: comparison of optical side effects. Summit PRK-LASIK Study Group. Ophtalmology. 2000;107(5):925.
[25] Rajan MS et al. A long-term study of photorefractive keratectomy; 12-year follow-up. Ophtalmology. 2004;111(10):1813.
[26] Pérez.Santonja JJ, Sakla HF, Alió HK, Contrast sensitivity after laser in situ keratomileusis. J Cataract Refract Surg. 1998;24(2):183
[27] Ransohouff DF et al. Prophylactic cholecystectomy or expectant management for silent gallstones. A decision analysis to assess survival. Ann Intern Med. 1983:99(2):199.
[28] UpToDate: Approach to the management og gallstones. Accessed 2019.05.06.