ALF MAGNE HORNELAND
Different people in different contexts interpret the term ‘risk’ differently. Different business areas have different definitions.
One definition of risk in general that also covers the aspects of medical selection is that Risk is the potential of losing something of value[1]. We will use this definition in relation to medical selection. The ‘something of value’ will be interpreted in a context regarding the direct effect on crew, ship, operations and the seafarer, indirectly also on the effect on liability and finances of ship operations and incidents that occur.
In Table 1 below, we mention some examples of different risk types.
Risk type | Related to |
Health risk | Likelihood of falling ill, getting a relapse of chronic or relapsing-remitting illness, and the seriousness of that incident, from little consequences to death |
Financial risk | Likelihood of losing financial values and the size of the loss |
Safety risk | Likelihood of being exposed to something threating one’s safety and the size of the danger |
Security risk | Likelihood of being exposed to hostile or criminal actions, and the consequences if it happens |
Table 1: Examples of risk types in medical selection. | |
It should be obvious that risk is not the same as probability of falling ill. Risk also relates to the seriousness of the consequences of an actual incident. The potential of losing something of value includes both the probability of the incident and the consequences of it.
C.8.7.1 The definition of risk
‘Risk’ is more than ‘probability’, or, said in another way:
The ‘potential of losing something of value’ is more than the ‘probability of losing something of value’.
In a similar way, we could say that ‘risk’ also is more than ‘consequences’.
In a simplified way, we could look upon risk as a product of likelihood and consequences, i.e., the potential loss is equal to a product of likelihood and consequences (Figure 2).
RISK (POTENTIAL LOSS) = LIKELIHOOD (FOR INCIDENT) X CONSEQUENCES (WHEN INCIDENT OCCURS)
Figure 2: Relation between risk, likelihood for and consequences related to a medical incident
C.8.7.2 Likelihood
The likelihood for a medical incident to occur, is often described in terms like ‘very low’, ‘low’, ‘negligible’, ‘inconspicuous’, ‘considerable’, ‘moderate’, ‘high’, ‘very high’ etc. We have no guarantee that different individuals have the same interpretation of this verbal grading of likelihood. In my experience, there is a considerable variation in understanding of the term ‘low likelihood’ from one to ten percent likelihood per year, which could lead to misunderstanding between specialists and approved medical examiners.
A first step towards a more accurate assessment and avoidance of misunderstandings is to agree upon a definition of terminology regarding likelihood.
C.8.7.3 Likelihood in the ILO/IMO Guidelines
The ILO/IMO Guidelines use this definition when discussing asthma[2], but do not apply this definition to all medical conditions:
- Very low: recurrence rate less than 2 per cent per year;
- Low: recurrence rate 2–5 per cent per year;
- Moderate: recurrence rate 5–20 per cent per year
The group ‘moderate’ may be valid for a clinical purpose. In relation to safety risk at work, we probably would regard 20% likelihood per year as a high likelihood. Hence it would be worth considering to introduce a ‘high’ recurrence rate for such likelihood.
Definition of likelihood
The Norwegian regulations, based on the IMO/ILO guidelines, take one more step in defining likelihood. The regulations generalize the definitions used for asthma in the IMO/ILO guidelines, and split the ‘moderate’ category in two, namely ‘moderate’ and ‘high’. These definitions apply to all conditions where likelihood can be estimated. For medical selection purposes, a likelihood >10% per year is regarded as high, and we therefore have applied the following definitions of likelihood in general[3]:
Verbal term of likelihood | Corresponding likelihood rate in percent per year |
Very low | Less than 2 per cent per year |
Low | 2-5 per cent per year |
Moderate | 5-10 per cent per year |
High | More than 10 per cent per year |
Table 2: The definition of verbal terms regarding likelihood, (NMA Health Regulations) | |
It would be advantageous to the further development of medical selection that all involved parties agreed to one definition, and we recommend the definition mentioned in Table 2. It is however not possible for doctors working with medical selection to specify how clinicians and epidemiologists structure their studies regarding risk bands. We probably will have to live with the differences, and interpret clinical data as good as we can when using them in a selection context.
C.8.7.4 Consequences of medical incidents vary in relation to job position and tasks
The probability for getting a common cold could be equal to that of getting a myocardial infarction (MI) in a given situation. The consequences, however, would be different. Setting a specific cut-off point for likelihood equal for all medical conditions therefore would make no sense.
The risk consequential to a catering crewmember getting an acute MI is not as big as the risk related to the same happening to a solo navigator manoeuvring a fast passenger boat with 150 passengers in littoral waters. Setting a specific cut-off point for likelihood equal for all job positions on board therefore would make no sense.
C.8.7.5 Medical incidents as triggers for chain reactions
The actual incident could serve as a trigger for a chain or cascade reaction. Such a reaction will start with the seafarer, but could include other crewmembers, the ship’s operation, a TMAS[4] on shore, a SAR[5] service, the port of call, the recipient of the goods carried on the ship, the ship operator, a manning agency, a hospital and a repatriation service. It also involves financial loss related to the above for the ship-owner, the operator, a manning agency and an insurer as well as the outcome for the seafarer, which sometimes is with sequelae. Hence those incidents that are most likely to trigger a complex chain of consequences are a priority for intervention as compared with incidents that are self-limiting and easily dealt with on board.
Figure 2 illustrates the cascade reaction that often follows a medical incident in a seafarer. It is obviously not restricted to the medical incident. The consequences are diverse.
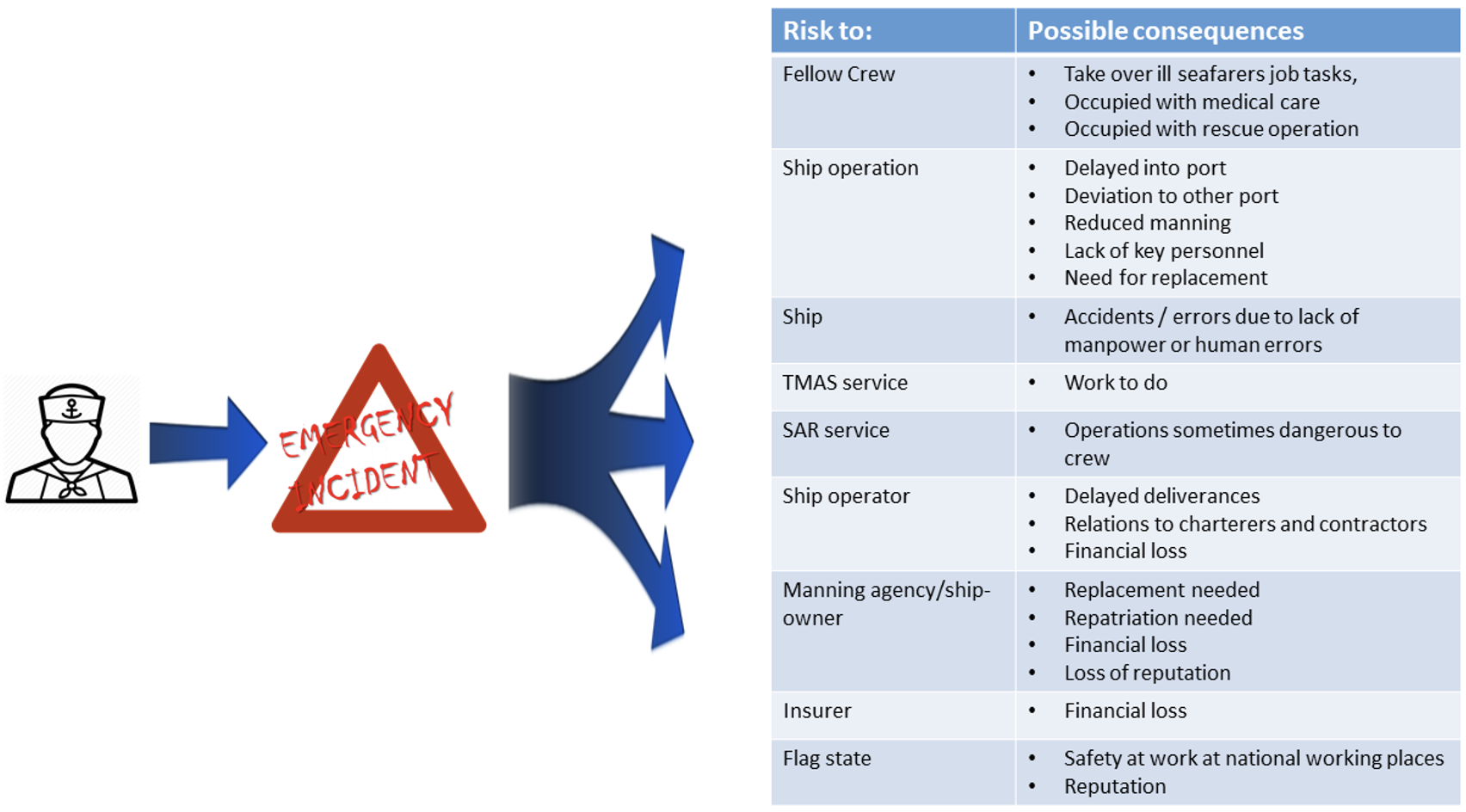
Figure 2. The cascade reaction after a medical incident.
References
[1] Kungwani P. Risk Managements – An Analytical Study. IOSR Journal of Business and Management (IOSR-JBM) e-ISSN: 2278-487X, p-ISSN: 2319-7668. Volume 16, Issue 3. Ver. III (Feb. 2014), PP 83-89
[2] ILO IMO Guidelines on the medical examination of seafarers, Sectoral Activities Programme ILO/IMO/JMS/2011/1, Appendix E, footnotes to the table, page 43.
[3] Regulations of 5 June 2014 No. 805 on medical examination of employees on Norwegian ships and mobile offshore units, Appendix E – Health requirements for common medical conditions, footnotes ii
[4] TMAS = Telemedical Maritime Assitance Service – often called Radio Medical Service.
[5] SAR = Search and rescue