TIM CARTER
A.1.2.1 Introduction
Knowledge about the health of seafarers has developed over the last few centuries. Particular problems or concerns have led to the collection of information and its use to plan methods for prevention. An early example of this was scurvy and its prevention by dosing seafarers with lemon or other citrus juice. There had long been suspicions that fresh fruit and vegetables prevented the condition and a study in the British Navy by Lind in 1747 provided some scientific support for this. It took a further fifty years for the navy to introduce lemon juice as both a preventative method and a means of treatment. It was to be over one hundred years before lemon juice was used effectively on merchant ships. Further information on the fight against scurvy is available in Ch 2.3.3.1. Similar examples can be cited in relation to infectious diseases such as smallpox and tuberculosis as well as for chronic conditions such as arterial disease and noise induced hearing loss.[1]
A.1.2.2 Quality of information on health risks
The previous section outlines a model for considering the state of knowledge on seafarer health risks and their management. On review of the available studies up to 2011[2] [3] , most were derived from information from one of the forms of healthcare contact shown in Figure 1. There is a weak information base derived from rigorously planned prospective studies on seafarers’ health. Such studies have the advantage of defining an at risk population in advance and then following their subsequent patterns of health using pre-set diagnostic criteria. They have formed the basis for many of the most important and definitive findings on health risks, for instance in onshore occupational health.
Specific issues in data collection
The definition of at-risk populations among merchant seafarers and in fishing has been one of the continuing limitations for epidemiological studies in this group for many years. Present day patterns of global recruitment on short term contracts have made this worse and in the fishing sector, non-standard conditions of employment, for instance on a profit sharing basis, make for similar problems. By contrast, the numbers serving on military ships and their demographic details are normally carefully recorded and they have ready access to a good standard of co-ordinated healthcare. This means that from the initial studies of scurvy in the eighteenth century onwards it has been possible to conduct rigorous investigation on health risks in the navies of the world.
However, naval, merchant shipping and fishing populations all share one common problem in terms of risk estimates: they spend their time in three different settings. The risks while at sea, while in port and while on leave are different. Any truly definitive study needs to look at the time spent in each setting and, indeed to look at the fine detail of each seafarer’s activities in each setting. At sea they will be exposed to different risks depending on their job and the trade the ship is engaged in. In port, risks will depend on freedom to go ashore, contacts with diseases, especially infections that are endemic or epidemic there and injury risks from motor vehicles and violence. On leave, they will lead their traditional lifestyle and be open to its associated risks.
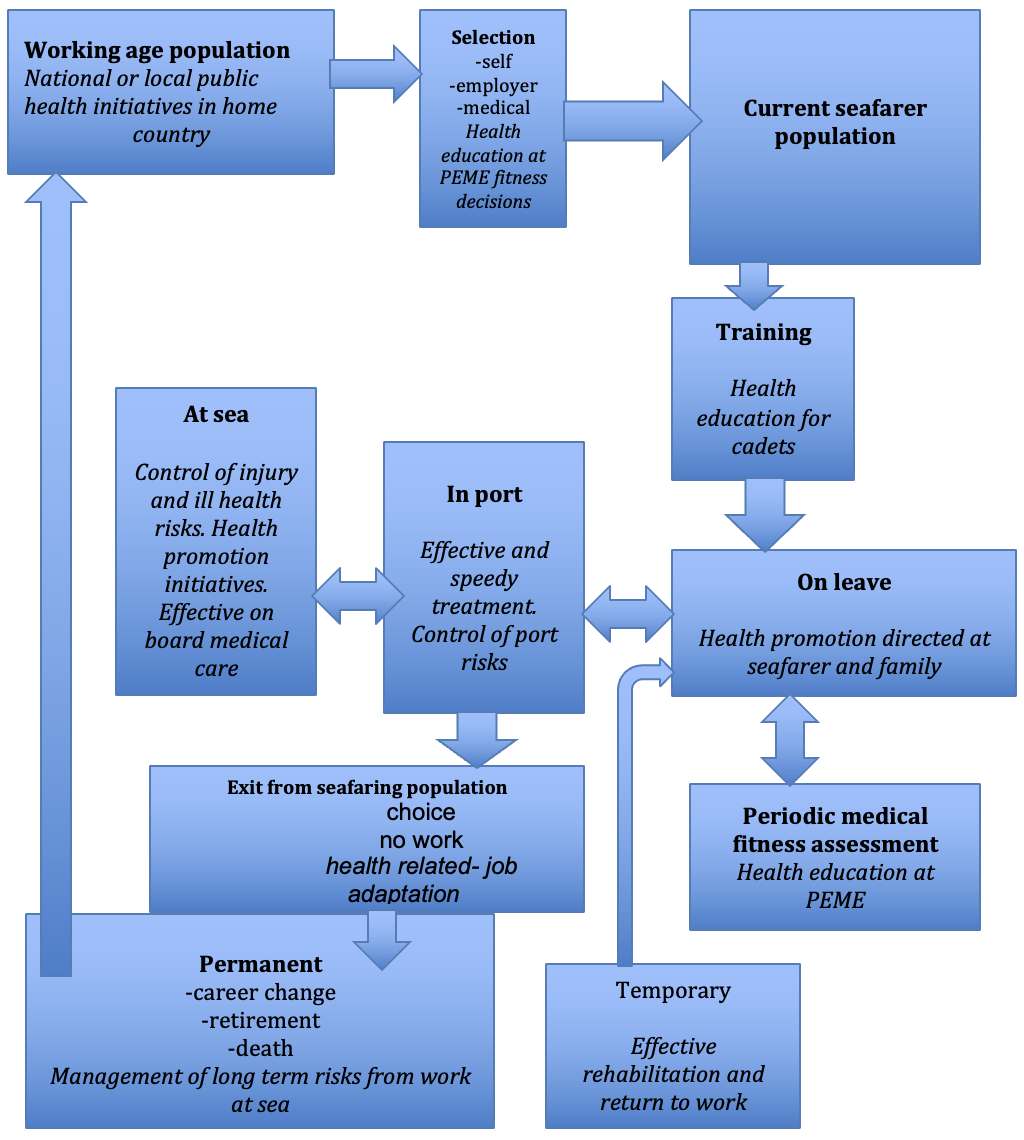
To date the knowledge base on seafarers’ health, with the exception of that on those serving in navies, is far from perfect. Nevertheless, it has provided the basis for setting some priorities for intervention within the range of settings where prevention is practicable. (Figure 2).
A.1.2.3 The effectiveness of health related interventions
Figure 2. Scope for health related interventions in seafarers
[1] Carter T. Merchant Seamen’s Health 1860-1960: Medicine, Technology, Shipowners and the State in Britain. Woodbridge: Boydell Press 2014.
[2] Carter T. Mapping the knowledge base for maritime health: 3. Illness and injury in seafarers. Int. Marit. Health 2011;62,4:224-235. https://journals.viamedica.pl/international_maritime_health/article/view/26161 Accessed 31 Dec 2019.
[3] Carter T. Mapping the knowledge base for maritime health: 4. Safety and performance at sea. Int. Marit. Health 2011;62,4:236-244. https://journals.viamedica.pl/international_maritime_health/article/view/26162 Accessed 31 Dec 2019.
Most of the available evidence on the effectiveness of interventions comes from time trends in frequency of disease or injury before and after such interventions. Just as for risk assessments, the quality of information on the effectiveness of health interventions is complicated by the different settings in which seafarers spend their time (Figure 2).
When an intervention can take place in a single setting, for instance the prevention of on board injuries or the control of an infection in a port area, and the effects are short term, the evaluation of effectiveness is straightforward. However where risks are spread over several settings, for example, those contributing to arterial diseases such as myocardial infarction or stroke, then both the planning of effective interventions and their evaluation are more complex.
This is a particular problem in relation to aspects of mental health, where risk factors may include personality, home circumstances and the demands of work on board and the consequences in terms of distress or ill health are difficult to quantify.
The ideal approach to the evaluation of interventions is a well-designed experimental study, similar to the randomised control studies used to assess the effectiveness of medications. This form of investigation is rarely feasible in the maritime setting and so planned interventions have to use less rigorous methods, such as using different populations of seafarers, some given the intervention and others with no intervention as comparison groups. Time trends before and after treatment are also used, as are natural experiments where studies take advantage of differences in exposure to presumed risks that are found in different parts of the seafaring population. The methods used to assess all forms of intervention are similar to those used when assessing risk: prevalence or incidence rates for the condition being studied. Well defined diagnostic criteria are needed and have to be applied consistently in all groups used for comparison.