A.1 Introduction
- Details
-
-
-
TIM CARTER
Securing good standards of maritime health is dependent on an adequate scientific underpinning of practice.
This is done by:
1. Analysis of information on the nature and scale of risks present. Important risks include
Or,
2. Evaluating the scope to reduce the impact of such risks by effective intervention. Interventions are commonly based on
Historically there has only been a limited evidence base on maritime health risks and on the effectiveness of interventions. This is a consequence of
Figure 1. Sources of routine medical information on seafarers
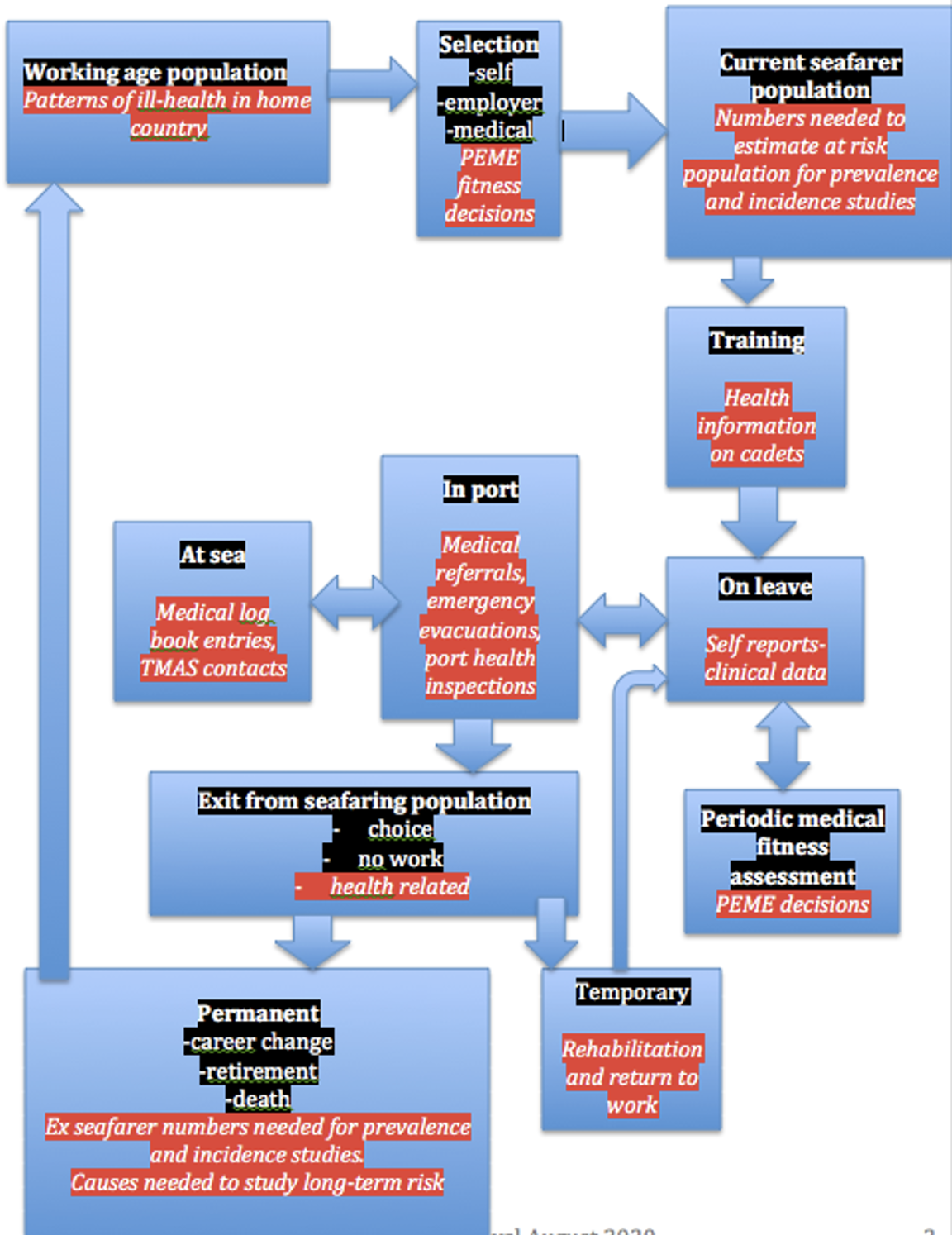
Maritime health risks and the effectiveness of interventions to control them can be investigated by methods similar to those used in other settings. Most involve comparisons between groups of people to identify differing levels of risk or different outcomes from intervention. In doing this it is always important to recognise that seafarers are a group that is both self-selected and selected by employers by means of medical examinations prior to employment. They are also a survivor population, with some people dropping out, either by choice or because they are forced to do so, as per Figure 1. This means that the working population of seafarers is likely to have a lower level of risk from illness than the general population, but also that long-term risks may be underestimated because those affected by them no longer work as seafarers.
Routinely collected information has been the main source for investigations of seafarers’ health risks. Such information arises from situations where a seafarer encounters a healthcare or administrative system that holds records. (Figure 1) Such sources often suffer from a lack of standardisation and consistency. Analysis is based on a range of techniques that are similar to those used for disease investigation on shore, but the complexity of sources of information and of seafarers’ patterns of work and leisure can make analysis more complex.
Key research question for each method in itallics
Have any unusual events/cases been identified or specific problems with case management noted?
Open to many biases depending on observer location, experience and interests. A major way for new problems to be identified and failures to control to known risks becoming apparent.
What is the relative frequency of different problems in the group studied? Diagnostic criteria needed. Biased by the setting in which the series is compiled. Increased relative frequency in some diagnoses may reflect not a real increase but simply a reduction in others. Sufficiently valid to show excesses of rare diseases, but not to give reliable information on more common conditions.
Case series of incidents or accidents can provide a similar form of evaluation of relative frequency and may show the role of health related impairments as contributors to accidents.
Are those with a particular medical, social or risk exposure history over-represented among those presenting with the condition being studied?
A case series may form the basis for a more formal case/control investigation. This can be done to study the history of exposure in those with a specific condition to see if there is a link. Cases of the condition are identified and matched with other people (controls) who do not have the condition but are demographically similar. Information on patterns of exposure is compared in cases and controls.
What is percentage of those at risk who have the condition at a point in time? Information is needed on the population from which the cases come to calculate this. Provides an absolute measure at a point in time, but prevalence rates depends on both the frequency and duration of the condition. At sea the population base may be the total number of crew/passengers on a ship, but onshore the difficulties in estimating the population of seafarers have been a major problem.
What is the rate at which new cases of a condition develop over a period of time?
Information on the total population is needed. The numbers of new cases are counted and their rate over a set period is calculated. Death, because it has to be determined for legal as well as medical reasons has been the event most commonly studied. The need to study chronic conditions such as pulmonary tuberculosis led to the collation of information from multiple sources to derive an estimate of the numbers of merchant seamen.
Because it is costly and needs to be done over a period of time, this approach has not been used for widespread morbidity studies in seafarers, and incidence studies on non-fatal illness have been limited.
Is the frequency, prevalence or incidence of a condition changing?
Trends can provide a natural experiment indicating changing patterns of disease or the effectiveness of intervention. Any of the above methods of study can show trends, but prevalence and incidence investigations will provide sounder information than anecdotal reports or case series.
These are rarely feasible in the maritime setting. They form the basis for investigations of the effectiveness of different treatment options, where individuals are allocated at random to one of a set of alternative treatments.
Can the pattern of illness in onshore populations be used to estimated risks to seafarers?
Onshore populations are both larger and easier to study. Results can be extrapolated to identify priorities for intervention in seafarers.
As shown in Figure 1, information on seafarer health can be collected in a range of settings. These include the following.
The prevalence and incidence of medical conditions can be calculated, using the total number of examinees as the denominator. Results are biased as, after the first examination, they come from a pre-selected population. Those with serious health problems will not present for an examination to determine their fitness to continue work.
Impairing illness or injury and deaths will be recorded. Apart from deaths, these sources have rarely been used. Landing an ill seafarer in port may be recorded, both for legal reasons to ensure repatriation and as part of clinical records.
Since the 1920s, records of radio medical advice to ships have had the potential to provide an additional source of information and a few case series are available. They may be biased as they depend on the decision of the master to seek advice.
Hospitals and clinics have been an important source of case series on acute illness. Much of their caseload will be acute illness. Ships, particularly those with surgeons, may have records of those sent ashore for treatment. Those concerned with repatriation are another source.
Seafarers may be identified by occupation in hospital records, on death certificates and on census returns. These sources can provide information on illness and death in those who are not currently working or who have retired. Biases include occupation from another job taken before retirement and lack of information on work at sea. In some countries, social security records contain details of service and of disabilities, while in others similar information may be available from pension funds.
The collection of health information for its own sake is pointless. Its value lies in its usefulness in reducing risks and improving interventions. Such uses include:
Information on patterns of illness and accident at sea and data from onshore populations can help to shape the criteria used for determining fitness. Employers’ concerns, which focus on the economic consequences of loss of a crew member and the costs of repatriation can differ from those of maritime authorities who are concerned for maritime safety and sometimes for decent working condition or those of seafarers and their trade union representatives who are keen to maintain members in work. The principles and practice of the use of medical examinations to determine fitness to work at sea are considered in chapter 4.8.
Includes determining the training requirements for officers in first aid and medical care. Also the requirements for medications, medical equipment, facilities and the contents of the ship’s medical guide, as well as the availability of radio medical advice. The development of all these facilities has been incremental; sometimes based on studies of illness at sea, more often on anecdotal information. Recommendations for change have usually been informed by developments in health care practice ashore rather than information gathered from seafaring populations.
The reasons for ceasing to work prematurely can be important in determining priorities for prevention of both general and work related diseases, as can information on disability or early death during retirement. Mortality information on seafarers and the findings from medical fitness examinations, social security sources or pension funds can all contribute.
Many health-related interventions have been underpinned with regulations or guidance. Sufficient evidence may be relatively easily obtained for injuries and specific acute diseases. Similar evidence on long-term disease is costly to collect and analyse.
Continuing collection of the sort of information that has been used to make the case for intervention will enable its effectiveness to be monitored. For instance, data on the frequency of scurvy, TB, malaria and venereal disease all confirm the success of the interventions that were made.
JAN SOMMERFELT-PETTERSEN AND TIM CARTER.
CONTRIBUTIONS FROM BOB BRIDGER AND MARGARETHA HOLENSDOTTER LÜTZHÖFT (MARPOL)
‘Shipping is perhaps the most international of all the world’s great industries and one of the most dangerous’.
Humans are naturally land animals. To be at sea is to be away from the environment in which we evolved and in which most people live. People may be at sea to work in maritime transport, fishing or specialist roles, as passengers, or pursuing leisure activities such as yachting.
The maritime environment may impose risks on them, including illnesses or injuries. It may also make demands on them, mostly relating to the tasks that workers perform, but some, such as remoteness from medical care, are relevant to everyone at sea. Travel itself may lead to risks from climatic extremes and from exposure to novel infections. Isolation and the work demands within the maritime setting can threaten wellbeing.
The recognition, evaluation and management of the risks and demands of being at sea are all components of maritime health. A range of disciplines is involved in identifying, preventing and managing the risk and thus ensuring that maritime work and leisure activities can be fulfilling while minimising adverse health effects. Disciplines include designers, engineers and managers as well as professional practitioners in medicine, psychology, occupational safety and health and related subjects.
Maritime health professionals require certain specialist skills in addition to those skills required for working ashore, including knowledge of the maritime living and working conditions. Practitioners have an important part to play in identifying health risks on board and in recommending ways of minimising them, usually in collaboration with other disciplines. To do this they may work as national or international policy makers, as company or trade union advisers, or as independent practitioners. It is important that they work within a framework of ethical standards such that their first duty is caring for the health of all who go to sea. More information on the ethical aspects of maritime health is available in Ch 2.9.
Maritime medicine is, in its essence, a global practice and historically, it was the start of international medicine. Maritime medicine comprises all the medical sciences relevant to sailors and their workplaces as well as to ships, harbours and docks and practitioners need to have clinical skills in the assessment of fitness and an understanding of the practicalities of delivering emergency treatment at sea. They may work ashore or sometimes on board a ship. There is not a clear, easy or precise definition of maritime medicine, but it can be described as
a discipline of medicine that is practised outside medical institutions. The patient is often treated on a ship in the middle of the ocean. The ship as a workplace is seldom at rest. The ship will not only roll and pitch, but sail in many, sometimes hostile, environments; physically, climatically and culturally.
The ship is more than a workplace that moves. It is at the same time, a home and a place for leisure. The ship is a 24-hour society, often with representatives of many different cultures on board and long periods of isolation from loved ones, friends and family. Ships are also isolated in the sense that what is not taken on board will not be available. Another special feature is that medical personnel do not usually practise medicine on board - non-medical personnel with very limited education in first aid and medical treatment deliver care on board the majority of ships. The patient will be a colleague and very often first aid is not enough, prolonged treatment is required because evacuation is impossible at that time. From a legal perspective, the ship is strange, complex and globalised. International conventions often provide minimum rules and regulations, national rules and regulations apply according to flag and, when the ship literally sails to different national legal systems, unexpected and dynamic legal challenges can arise. More information on the regulation of the shipping industry is available in Ch 2.10.
The institutional anchor for maritime medicine is fragile. In most university hospitals, there are departments, consultants and professors covering almost any and all medical specialities, except maritime medicine.
Maritime medicine is special and so extreme that it is necessary to consider the interface between health, safety and risk. All on board are dependent on the safety and integrity of the ship thus safety is sometimes more important than health. It is important to ask which focus will be most efficient, medical treatment or medical prevention. From a public health perspective, the issue is important, and the historical examples given in this chapter will stress the point.
Knowledge of maritime medical history makes it easier to understand maritime medicine in general and today’s challenges in particular. The history of maritime medicine is long and will not be presented chronologically, but thematically in four themes - the sea, the ship, maritime medicine and the sailors.
‘The complex and all-consuming Ocean feeds man, but also feeds upon men. The flat calm that gently digests my troubles is capable of violent turbulence and of enough gluttony to chew up and spit out vessels of the strongest steel. Often swallowing men and ships
whole…’[1]
Everyone with a connection to the sea has heard the saying ‘The sea gives, and the sea takes away’. The sea can be a dangerous place, and many have found a wet grave. The sea covers more than 70 % of the surface of the earth and slowly man has learnt to be able to travel over the sea in safer and healthier ways.
From a Norwegian perspective, up to 90 % of all export from and import to Norway takes place on ships and shipping, fisheries and the pumping of oil and gas from the seabed are central to the Norwegian economy and society. The sea is an important factor for life and health and thus of central importance in maritime medicine. Internationally around 90 % of all goods transported are transported by sea. [2]
Prehistoric peoples crossed seas as settlement spread around the globe and by classical times, the Mediterranean was the theatre for both regular trade routes and for occasional naval battles. Similar patterns were seen around the coasts of Asia, while the navigational achievements of Polynesians in settling on remote islands in the Pacific Ocean took place around the same time. Viewed from a Norwegian perspective the recorded history of maritime activities is a long one. Around the year 1000, Leif Erikson and his crew (ca. 973 - ca. 1020) sailed westward and became the first European to set foot on the American continent. They sailed close to the coasts, did not stay for extended periods at sea and there is nothing to indicate any health problems during the voyage. Several sagas document the trip[3], but it was disputed for a long time until proven by archaeological excavations at L’Anse aux Meadows in Newfoundland in 1960.[4] Leif Erikson demonstrated the possibilities of exploration and long travels at sea and in time these became a substantial challenge to the health of seafarers.
The sea opens a world of challenges and possibilities. Dry fish has been a very important industry since Viking times. Dry fish is usually dried cod[5] and drying fish was the preferred method for conservation until affordable salt from Southern Europe became available in the 16th century. Clip (salted and part dried) fish then became an alternative. In the 9th century, dry fish was the most important export commodity from Norway and in Egil Skallagrimsson’s saga[6] we can read about the headman Torolv Kveldulvsson’s export of dry fish from North Norway. In 875 he sailed with cod from Lofoten to England “to buy clothes and other necessities”[7] In the 10th century the dominant position of Bergen and its merchants was established, based on this export business. Dry fish was an important source of food both on board and on land.
From around 1300 onwards the Atlantic facing nations of Europe, first Spain and Portugal and then later Britain, France and the Netherlands, embarked on oceanic voyages, discovering new lands, often plundering them and fighting with one another over the spoils.
In 1493 Pope Alexander VI (1431-1503) drew a line of demarcation 550 km west of the Cape Verde Islands and gave control of territory to the west of the line to Spain and east of the line to Portugal. Portugal contested the decision and in 1494, after negotiations with Spain, the line was moved to 2055 km west of the Cape Verde Islands according to the Treaty of Tordesillas. Portugal used this treaty when Pedro Alvares Cabral (1467-1520) discovered Brazil for Portugal in 1500. No other countries accepted this treaty and many countries started claiming different parts of the ocean. Denmark-Norway laid claims to the North Sea, Kattegat and the Baltic Sea.[8] In his book Libre marum (1609), the Dutch thinker Hugo Grotius (1583-1645) gave his arguments for the view that the sea was free for all. The arguments were most useful for Dutch economic interests and the successful expansion of the first multinational company in the world - the Vereenigde Oost-Indische Compagnie (VOC). The English did not accord and demanded sovereignty over the waters around their island. In Mare clausum (1635), John Selden (1584-1654) argued that the sea could be occupied in the same way as land areas. In his ‘De Dominio Mmaris of 1702, Cornelius van Bynkershoek (1673-1743) contended that a country could claim sovereignty as far out from the coast as a canon could shoot. This idea became the internationally accepted principle of a three-mile limit defining a country's territorial waters.
Freedom of the seas was gradually accepted as a part of international law. Today, these rules are incorporated in the United Nations Convention on the Law of the Sea, UNCLOS, of 1982. For ships sailing on the open - and free – seas, the principle is that flag state regulations apply. More information on the law of the sea is available in Ch 2.10.
Techniques of navigation improved as voyages lengthened. Methods for taking sights on the sun and stars were developed. Charts plotting water depths and coastal profiles were produced, both in Europe and in Asia, where for a short period Zeng He, a Chinese admiral explored widely.
One of the most serious threats to life at sea is shipwreck. On October 22nd 1707, four naval ships were wrecked on the Scilly Islands, southwest of Cornwall off the English coast. The fleet of 21 naval ships was under the command of Admiral Cloudesley Shovell (1650-1707) and he perished, along with the complete crew of his flagship, a total of 800 men.[9] The reason for the mishap was navigational, they had not managed to estimate their position correctly. Subsequently, in 1714 the British Parliament passed the Longitude Act and a Board of Longitude was established. The Board announced a reward of £20 000 to anyone who could find a reliable method of determining the longitude at sea, equivalent to £2.89 million in 2018.[10]
Many tried to find a solution to the problem. One method that worked was astronomical, but it was too difficult for navigators to use. The watchmaker John Harrison (1693-1776) solved the problem by inventing a very accurate clock, a ships’ chronometer, to estimate the longitude. The Board of Longitude never gave him - or anybody else - the award. The issue was hotly debated for a long time, and when Harrison had turned 80 the Parliament awarded him £8 750 for his work.[11] Harrison’s chronometer solved the problem and was a huge step forward in navigational safety. His invention has saved the lives of countless seafarers. The Board of Longitude was dissolved in 1828 because its purpose had been fulfilled.[12]
Since this time, navigational aids have continued to improve with the publication of detailed charts, the building of lighthouses and placing of buoys, culminating in digital charts and global positioning satellites that enable positions and courses to be plotted to within a few metres.
One of the great risks of seafaring is bad weather. Experienced sailors have respect for the weather, but a storm can surprise those already at sea. A weather forecast is a meteorological prognosis on the upcoming weather. Thanks to Samuel Morse,[13] (1791-1872) and the invention of the telegraph in 1837, it became possible to collect many real time observations of the weather in a large area and this increased the quality of weather forecasts. Around the same time, the Irish hydrographer and Admiral, Francis Beaufort[14] (1774-1857) invented a scale to standardise wind measurements. At The Battle of Sevastopol in 1854, an unforeseen storm destroyed many French and British naval ships.[15] This tragic event encouraged the Admiral to do more and he organised the first successful network of ground observation posts for weather in the mid-1800s.[16] He also influenced the English Vice Admiral, hydrographer and meteorologist Robert FitzRoy (1805-1865)[17] who developed a special type of barometer and distributed the instruments to several ports. In 1862, FitzRoy organised the first storm warning weather service based on information collected through telegraph messages.
The Norwegian physicist Vilhelm Bjerknes (1862-1951) developed a cyclonic model to explain atmospheric air movements in the early 1900s. He discovered the physical explanation for polar fronts and introduced the concepts of warm and cold fronts. His research group, called the Bergen School, and the models they developed are still accepted and in general use. Bjerknes is described as the father of weather forecasting.
Improvements in meteorological science and in communications, starting with the deployment of weather ships and balloons carrying instruments into the upper atmosphere and now complemented by satellite observations and computer modelling of air movements have improved the predictive value of forecasts. But major weather events such as hurricanes do still put ships and crews at risk.
Avoid landing on a stormy day
Figure 1 Landing ships putting cargo ashore on Omaha Beach, at low tide during the first days of the operation. Photo: https://commons.wikimedia.org/w/index.php?curid=2263487 |
The Allied invasion of Normandy was originally planned to start on June 5th 1944. It was the largest amphibious operation ever conducted. The Norwegian meteorologist Sverre Petterssen (1898-1974) was one of the experts asked to do the important weather forecast for this risky amphibious operation. He concluded that the weather would be too bad by using the methods of the Bergen School.
“Petterssen managed to pull the brake on June 4th … and he was right. On the 5th of June a heavy storm ravaged the channel”.[18]
The Germans expected bad weather and relaxed their readiness. Petterssen convinced General Dwight D. Eisenhower to postpone the operation one day. There is substantial disagreement about the weather forecasts prior to D-day. Three different meteorologist centres produced forecasts[19], using the same set of observations, but varying in methodology. One day before the invasion was planned Petterssen managed to convince the Admiralty to support his position and to postpone the invasion. The Americans disagreed. Stagg summed up the recommendations, two against one, and presented the majority view to Eisenhower. The invasion was delayed one day.[20] [21]
President John F Kennedy once asked Eisenhower why the invasion of Normandy became a success. His reply? ‘Because we had better meteorologists than the Germans’.[22] The invasion, Operation Overlord, was one of the biggest military operations ever conducted. 24 000 paratroopers were dropped over the target, 156 000 soldiers were transported on around 700 ships and 5 400 fighter planes, and 3 000 bombers flew 14 000 sorties the first day.[23]
For sailors the ship is their world. For the ship owner the successful completion of the voyage is essential. For both, the safety of the ship is paramount. These truths have remained, but ships have changed markedly over the years.
Shipbuilding was a skilled trade in the ancient world and wood was the chief raw material. Wooden ships became larger and more seaworthy as voyages lengthened and building techniques improved. Cargo carrying ships needed maximum cargo capacity, those carrying urgent and valuable goods needed speed, while ships designed for fighting needed the speed, manoeuvrability and the capability to ram, board or later fire at the enemy.
Until the late eighteenth century wood remained the main construction material and propulsion came from the wind on sails or human muscles pulling oars. The development of the steam engine and improvements in iron and then steel making led to a massive transformation in ships between 1800 and 1900. They became larger, faster and able to steer predictable courses to a predetermined timetable. While the risks of crew death and injury were less than on sailing ships, the increase in speed and size, and hence crew and passenger numbers made the worst-case disaster scenario ever greater.
The ocean liner RMS Titanic collided with an iceberg on April 25th 1912 and disappeared from the surface three hours later. At the time, Titanic was the world’s largest ship and on her maiden voyage from Southampton to New York. She had 20 lifeboats launched with 705 people (of which 675 were women and children) and three pets. There were enough life jackets and when Titanic disappeared from the surface, around 1 500 persons were in the cold Atlantic. It was a quiet night and around zero degrees Celsius. Everybody in the sea perished from exposure and hypothermia.[24]
Figure 2 RMS Titanic departing Southampton on April 10, 1912. Photo: F.G.O. Stuart (1843-1923) - https://commons.wikimedia.org/w/index.php?curid=2990792 |
Because of this disaster, the first Safety of Life at Sea (SOLAS) convention was signed on January 20th 1914.[25] SOLAS requires, amongst other things, that all ships have enough space in the lifeboats for all passengers and that all ships always have an obligation to listen to radio.[26] This convention was the beginning of a new era of international collaboration on maritime safety.
The beginnings of similar international collaboration on maritime health can be identified. By 1920, many major maritime states had specified requirements for medical care at sea including fitness to work, medicines, a medical guide and training for officers. In the 1920s the Red Cross and the newly established International Labour Office, took several initiatives to promote the health of sailors. In Norway, the Red Cross asked Lieutenant Commander and doctor Harald Engelsen (1883-1954), then head of the Navy Bacteriological Laboratory, to take on this important work. In 1924, the general assembly of the International Red Cross passed a resolution tasking the Norwegian Red Cross to make an international medical guide for ships and a standardised medical chest on board all ships. If all ships had a medical guide and medical supplies on board, radio medical advice would be greatly simplified for all. [27]
Dr Engelsen presented the work done to the International Conference on Sailor’s Health in Oslo, Bergen and Trondheim in 1926. He presented an International Medical Guide for Ships along with a special set of medical code signals for use over radio. He also proposed a standardised medical chest for ships. This Norwegian medical guide for ships was translated into French, but getting the book internationally accepted by all nations was difficult. However, it was widely distributed and in 1927 it was authorised for use on all Norwegian vessels. At the same time the Norwegian Parliament decided to further the efforts to improve sailors’ health by donating the large sum of 200 000 Norwegian kroner to the Red Cross work for sailors At the Red Cross international conference in Tokyo in 1934, the International Medical Guide for Ships was recommended for all nations.[28]
Following World War II work continued and finally, in 1967 that the ILO, World Health Organisation (WHO) and the International Maritime Organisation (IMO), published the first edition of the International Maritime Guide for Ships. The second edition was published in 1988 and translated into more than 30 languages, the third edition was published in 2008.
Figure 3 The flag for "w" |
The aim of the International Code of Signals (ICS) is to ‘provide ways and means of communication in situations related essentially to safety of navigation and persons, especially when language difficulties arise.’[29]
ICS has a long history[30] and the signals can be sent in many ways, from using light to flags or radio. The code “W”, means ‘I require medical assistance’.
In 1930 a new version of the international code of signals was produced and passed by the International Radiotelegraph Conference[31] in Madrid in 1932. Because of Engelsen’s initiative for sailor’s health, the medical section was approved by the Office International d’Hygiene Publique[32] in Paris.
The oil tanker SS Torrey Canyon was wrecked just off Lands’ End in southwest England on March 18th 1967. The weather was fine. The wreck was attributed to a navigational error, the human factor was to blame.[33] The ship was large, 120 000 dwt, and the largest vessel ever to run aground.[34] Several attempts were made to save her, but on March 27th, the salvage party had to abandon their attempt because of poor weather.[35] After eight days the ship broke in two. To limit the oil spill from the huge ship she was bombed and eventually sunk by air assets from the Royal Navy. The cargo was crude oil and the spill polluted large areas in South England, the Channel Islands and Bretagne.
The accident with SS Torrey Canyon was the largest oil pollution disaster ever at that time and it led to the development of international conventions to combat oil pollution and institute contingency measures to limit the effects of oil spills. An International Convention for the Prevention of Pollution from Ships (MARPOL) was developed in 1973. Again, we see that serious accidents are necessary to change rules and regulations.
Admiral Richard Hawkins (c. 1562-1622) called scurvy ‘the plague of the Sea,[36] Scurvy is probably the disease that has killed more sailors than any other cause. Today scurvy is an extremely rare disease and most doctors have never seen such a patient. Scurvy is characterised by ‘… prominent cutaneous signs (petechiae, perifollicular haemorrhage, and bruising), gingivitis, arthralgias, and impaired wound healing, appearing within a few months of a vitamin C-deficient diet.’[37]
Scurvy became a common problem for explorers during the long voyages in the 15th century. With the exception of some Vikings 4-500 years earlier, the Portuguese were the first to encounter scurvy. Vasco da Gama (c. 1460-1524) left Lisbon with a fleet of four ships and 160 men on 8th July 1497. He sailed to find the new route to the east and he reached India. After a couple of months on board, scurvy appeared and da Gama lost over 100 of his 160 men to scurvy. No efficient treatment was known.
Only three years later, Pedro Alvares Cabral (1467-1520) described an efficient treatment for this terrible ailment in a travelogue. He stated that in Mombasa his scurvy patients got treatment and ‘the oranges made them well again’.[38] The solution to the problem was found, forgotten and found again, many times.
George Anson’s first circumnavigation
Commander George Anson (1697-1762) sailed from England with a fleet of seven ships in 1740. When he returned four years later, only 145 of the original crew of 1955 were alive. Around 1300 of more than 1800 deaths were caused by scurvy.[39] The expedition was viewed as one of the largest medical catastrophes in its time.[40] This was also the first time scurvy became a problem discussed in public.[41] The ship’s surgeon thought salt meat and laziness were to blame. The College of Physicians recommended vinegar against the illness and the Admiralty accepted their recommendation. Anson himself wrote a report, ‘Voyage Round the World in the Years 1740-44’, published in 1748 and it became so popular it was reprinted several times during the first year after its publication.
Figure 4 A portrait of Scottish doctor James Lind (1716–1794) by Sir George Chalmers, c 1720-1791. Photo: https://commons.wikimedia.org/w/index.php?curid=32922810 |
During the Seven Years’ War (1756-1763) out of a total number of 184 899 men, the British Royal Navy lost 1 512 (0,8 %) men in war and 133 708 (72 %) to illnesses[42]. Scurvy was the major cause of death.[43] Obviously there were a number of good reasons why the “the plague of the Sea” should be stopped. The problem was, it could not be solved because it could not be understood.[44]
James Lind and the world’s first controlled medical experiment
In 1746, the Scottish surgeon James Lind (1716-1794) signed on as a ship’s surgeon on HMS Salisbury. The ship had a crew of 350 men and that year they had a large outbreak of scurvy with more than 80 taken sick. Next year they again had an outbreak of scurvy and Lind conducted an on-board medical experiment. He isolated twelve sailors with scurvy and gave them all the same diet.[45] Then he divided the patients into groups of two and gave these groups different additional diets for 14 days. The six additional diets were
‘Two of these were ordered each a quart of cider a day. Two others took twenty five gutts of elixir vitriol three times a day, upon an empty stomach; using a gargle strongly acidulated
with it for their mouths. Two others took two spoonsful of vinegar three times a day upon an empty stomach; having their gruels and their other food well acidulated with it, as also the gargle for their mouth. Two of the worst patients, with the tendons in the L arm rigid, (a symptom none of the rest had) were put under a course of sea-water. Of this they drank half a pint every day, and sometimes more or less as it operated, by way of gentle physic. Two others had each two oranges and one lemon given them every day. These they eat with greediness at different times, upon an empty stomach. They continued but six days under this course, having consumed the quantity that could be spared. The two remaining patients took the bigness of a nutmeg three times a day, of an electuary recommended by an hospital-surgeon, made of garlic, mustard seed, rad. raphan. Balsam of Peru, and gum myrrh; using for common drink, barley water well acidulated with tamarinds; by a decoction of which, with the addition of cremor tartar, they were gently purged three or four times during the course.’[46]
Lind tells us that the two who got oranges and lemons swiftly became better and could take part in the nursing of the other patients. The two who got cider also improved and after two weeks
‘the putrefaction of their gums, but especially their lassitude and weakness were somewhat abated ... As to the elexir of vitriol, the mouths of those who had used it by way of gargarism [as a gargle] were in much cleaner and better condition than many of the rest, especially those who had used vinegar; but I perceived otherwise no good effects of its internal use upon the other symptoms ... There was no remarkable alteration upon those who took the electuary and tamarind decoction, the sea-water, or vinegar, upon comparing their condition, at the end of the forthright, with others who had taken nothing but a little lenitive [pain-killing] electuary and cremor tartare, at times, in order to keep their belly open; or a gentle pectoral [cough syrup] in the evening, for relief of their breast.’[47]
Lind concluded that ‘oranges and lemons were the most effectual remedies for this distemper at sea’. Lind started his experiment on 20th May 1747 and Professor of Public Health, Dag S. Thelle asserts that Lind’s experiment was the first ever, controlled experiment.[48] James Lind has been awarded the honour of being named the “father of naval medicine”[49] and 20th May has been named International Clinical Trials Day in his honour.[50] Maritime medicine has certainly made some positive impact outside the field of naval medicine.
Change of diet
The Royal Navy did not introduce citrus fruits into the diet of their sailors until many years later, in 1795 when navy surgeon Gilbert Blane (1749-1834) succeeded in convincing the Admirals to do so. When First Lord of the Admiralty, Admiral George John Spencer (1758-1834), visited the Royal Navy Hospital at Haslar in 1797, there was not a single patient in the hospital with scurvy. Usually they accounted for up to 50 % of the patients. Scurvy was defeated, the blockade against Napoleon was possible to carry through so Napoleon could be defeated - and the British sailors got the nickname ‘limeys’.[51]
Unfortunately, scurvy later reappeared and was a most feared disease in arctic expedition - a field where Norwegians were prominent.
Around 1900, two Norwegian doctors, Axel Holst (1860-1931) and Theodor Frølich (1870-1947)[52] became interested in beriberi, which ravaged Norwegian ships, but was seldom seen on ships from other nations. They suspected that the illness could have a connection to the sailors’ diet. They established an animal model using guinea pigs to study the effects of different diets, and, to their surprise, rather than developing beriberi, the guinea pigs got symptoms of scurvy on a diet of products from grain, but not if they added fresh cabbage or lemon juice to the diet. They also showed that animals already sick from scurvy could be cured by the same diet. Holst and Frölich concluded that scurvy was an illness of nutrition. At this time in history, the idea of nutritional disease was not yet invented. In 1907, they published their findings in the international Journal of Hygiene[53] and met a lot of opposition from colleagues who did not subscribe to any idea of deficiency disease or any theory of disease caused by nutrition. Poisoning and infection were causes that were much more popular at the time. They did not get any acknowledgement or prizes for their research and consequently moved on to other fields.[54]
Vitamins
In 1912, Casimir Funk (1884-1967), a Polish chemist doing research at the Lister Institute in London, presented an unusual hypothesis. He asserted that scurvy, pellagra, rickets and beriberi, all represented a class of diseases caused by deficiencies in the diet. The lack of certain nitrogen’s with the ‘amine’ structure caused each of these diseases. He called these structures vitamins (short for vital amines) and became the name giver for a new concept of vitamins as important substances in health.[55]
Ascorbic acid
The Hungarian Albert von Szent-Györgyi Nagyrápolt (1893-1986) managed to isolate ascorbic acid and identify the acid as vitamin C. He was awarded the Nobel Prize in 1937 for his important achievement.[56] The fight against the plague of the sea was finally crowned with victory.
During the efforts to salvage SS Torrey Canyon in 1967, there was an explosion on board the tanker and people from the salvage teams ended up in the water. Navy doctor and then lieutenant, Frank Golden was on duty at the nearby Naval Air Station. The Royal Navy search and rescue helicopter rescued the salvage team from the sea but unfortunately, Captain HB Stal died after he was hoisted from the sea. This sad fact frustrated Golden and he was even more disturbed by the lack of medical understanding of what happens when personnel are rescued from immersion in the sea. The knowledge on details around immersion in cold water was insufficient. Golden enlisted in a PhD[57] programme at the University of Leeds and the theme of his dissertation was the effect of cold immersion. His lifelong interest and effort in the field resulted in new and improved procedures for rescue from the sea and test procedures for maritime survival equipment.[58] Of special importance was his discovery that it is a huge risk to hoist people from the sea in a vertical position. Rescue from the sea must be made in a horizontal position to avoid possible deaths caused by post-immersion collapse. This form of death was mentioned as far back as James Lind[59] and the Second World War highlighted it.[60] Nevertheless, it was not until Golden’s effort that the procedures were both understood and changed.[61]
The maritime sector depends on competent and reliable seafarers. Maritime health interventions contribute to this in many ways, these require a range of technical, operational and clinical (medical and psychological) skills.
Figure 5 A sailor on his way to the doctor at the Norwegian Public Health Office in New York. Photo: Official Norwegain War Photo |
Some say that personnel are the most important resource. Sailor’s skills are important for the job they are doing. It is essential to have the right man or woman in the right place to ensure that the task is accomplished safely. Most accidents at sea seem to be a result of the human factor. Medical selection is one important tool to ensure that the sailor is fit for duty.
Medical selection is a tool used to get the right man or women in the right place at the right time. A prerequisite for successful selection is not only medical knowledge, but just as important, is the doctor’s knowledge of the workplace and the procedures used at work. When you add sailors with illnesses or injuries to the equation the seaman’s doctor must consider if the sailor is fit for work with the illness or injury, the assessment becomes even more complicated. Before deciding if the sailor is fit for work, the seafarer’s doctor should assess the risk for the ship, the risk for others and the risk for the sailor himself depending on the function, the job, the ship and the circumstances. This is a very complex matter and differs significantly from providing ordinary medical treatment.
There is a long history on the selection of sailors leading to present day practice, more information on which can be found in Ch 4.8.
The Navy made the oldest known health prerequisites for service at sea. In the 1600s, gunners in the Danish-Norwegian Navy had to be found seaworthy to be enrolled.[62] The Naval Academy of the Danish-Norwegian Navy was established in 1701[63] and after the separation of Norway from Denmark in 1814 a Norwegian Naval Academy was built in Fredriksvern.[64] A Royal Decree of 1816-12-23 laid down the regulations for the academy and these contained requirements for the cadet’s health and mobility. They demanded normal ability of speech, hearing and eyesight and if any cadet did not meet any of these standards, they should be dismissed.[65]
Civilian maritime health regulations started with requirements concerning normal eyesight, hearing and the absence of contagious diseases. For navigators and deck crew there was also a requirement for normal colour vision. The health requirements were gradually extended to include an assessment of the risk of getting ill and need for repatriation because of illness. The Insurance Company Skuld established a more comprehensive system for pre employment health examinations in cooperation with the authorities. The Skuld system started June 10th 1938.[66] During the Second World War the Norwegian Government in exile took over the Skuld system and established Norwegian Public Health Offices in relevant ports.
In 1946, International Labour Organisation passed a convention on medical examination of sailors.[67] The convention requires health examination before entering service and requires sufficient sight, hearing and absence of contagious diseases. See Ch. 4.8
During the Second World War, the Norwegian merchant navy was one of the biggest in the world and the Norwegian ship owners had invested heavily, especially in tankers. After the German attack on Norway on April 9th 1940, the government ordered all Norwegian ships to proceed to ports controlled by the allied forces. Norwegian ships outside Norwegian waters were organised into a single government shipping company called NORTRASHIP[68] and all of them sailed in support of the allied war effort. The sailors, around 35 000 men and some women, suddenly became a part of the war effort without ever being medically selected for this task. On the other hand, the merchant navy was Norway’s most important contribution to the allied war effort. In 1941, the British admiral Gerald Charles Dickens stated that ‘were it not for the Norwegian Merchant Marine, we might as well have asked Hitler for his terms’[69]
In addition, the merchant navy earned a lot of money and thus the Norwegian government in exile had substantial economic freedom during the war and a solid basis for the rebuilding of Norway after the liberation. On the other hand, the handling of the Norwegian wartime sailors after the war ended appears more like a public health disaster.
Post-traumatic stress
Hoffman conducted one of the earliest surveys of the health of wartime sailors in 1945.[70] He studied 155 sailors admitted to convalescent homes in America. He found 61 sailors with conditions assessed as due to war experiences. The symptoms were insomnia, jumpiness, tremor, vegetative dysfunction and depression. There were very few hysterical reactions. Hoffman also showed that most of the sailors got their problems after repeated exposure to trauma and not after single experiences.
Shortly after the Second World War, a Danish group of researchers under the direction of Dr Per Helweg-Larsen who studied concentration camp prisoners demonstrated a typical clinical picture the so-called KZ-syndrome.[71] The group had higher morbidity and problems with concentration, irritability, nervousness, depression, insomnia and headache. Some of them had immediate onset of symptoms while others developed symptoms later.
These investigations were among the earliest to identify the symptoms that are now widely recognised as characterising post-traumatic stress disorders.
Maritime health is in its essence both international and global. It cannot be sufficiently understood within a narrow medical perspective, but must include the technical, economic and cultural aspects of shipping. Solutions internal to the shipping industry or internal to individual nations cannot solve today’s challenges in maritime health. Problems cannot be solved in splendid isolation, but by international cooperation. Maritime medicine, unlike much specialised onshore clinical practice, includes care of the healthy and, as such, is close to public health and occupational health. However, when sailors get ill or injured or end up with late onset ailments, maritime medicine needs to include the relevant elements of all specialities of medicine.
International maritime health initiatives and cooperation must be based on sound and solid medical knowledge. Institutional competence in this field is scarce and there is a need for many more centres of maritime health and medicine to serve as anchors for maritime medicine practice and research. Shipping is one of the economic sectors with the highest mortality and morbidity, and more research is needed to guide efforts to further the health of the sailor and the whole maritime sector. This chapter has given some examples of successful and unsuccessful initiatives in the past; may the future developments make the lessons identified into lessons learned.
[1] Greenlaw, L. 2000. The Hungry Ocean. A Swordboat Captain's Journey. New York, Hyperion Books.
[2] https://www.ics-shipping.org/shipping-fact/shipping-and-world-trade-world-seaborne-trade/ Visited: 2021-10-06.
[3] https://www.britannica.com/place/Vinland#ref226391
[4] Ingstad, H. Et al. 2001. The Viking Discovery of America. The Excavation of a Norse Settlement in L'Anse Aux Meadows, Newfoundland. Checkmark Books.
[5] Kurlansky, M. 1998. Cod. A Biography of the Fish that Changed the World. London, Penguin.
[6] Full text available at https://sagadb.org/egils_saga.en Visited: 2019-03-27.
[7] Wikipedia; Stockfish https://en.wikipedia.org/wiki/Stockfish Visited: 2018-10-15.
[8] Store norske leksikon [Main Norwegian encyclopedia] https://snl.no/%C3%85pne_hav Visited: 2018-10-15.
[9] Wikipedia: Scilly naval disaster of 1707 https://en.wikipedia.org/wiki/Scilly_naval_disaster_of_1707 Visited: 2018-10-29.
[10] Wikipedia: John Harrison https://en.wikipedia.org/wiki/John_Harrison Visited: 2018-10-29.
[11] Ibid..
[12] Wikipedia: Board of Longitude https://en.wikipedia.org/wiki/Board_of_Longitude Visited: 2018-10-29.
[13] Wikipedia: Samuel Morse https://en.wikipedia.org/wiki/Samuel_Morse Visited: 2018-10-15.
[14] Wikipedia: Beaufort scale https://en.wikipedia.org/wiki/Beaufort_scale Visited: 2018-10-15.
[15] Wikipedia: Great storm of 1854 https://en.wikipedia.org/wiki/Great_Storm_of_1854 Visited: 2018-10-15.
[16] Wikipedia: Weather forecasting https://en.wikipedia.org/wiki/Weather_forecasting. Visited: 2018-10-15.
[17] Wikipedia: Robert FitzRoy https://en.wikipedia.org/wiki/Robert_FitzRoy. Visited: 2018-10-15.
[18] Njåstad, M. 2016. Slik blei norsk meteorologi verdsleiande. Bergen, På Høyden. http://pahoyden.no/2016/10/slik-blei-norsk-meteorologi-verdsleiande Visited: 2018-10-16.
[19] The Brits at Dunstable, the Americans at «Widewing» and the Admirality (Nilsen, Y. Et al. 2016. Vinden Dreier. Meteorologiens historie i Norge. Bergen, Scandinavian Academic Press; 237).
[20] Nilsen, 2016; 239.
[21] There has been substantial disagreement about what really happened in the days before the invasion. See the different viewpoints in Krick, IP. Et al. 1954. Sun, Sea and Sky. Weather in our World and in Our Lives. J.B. Philadelphia, Lippincott, 248 pp.; Stagg, JM. 1971. Forecast for Overlord. June 6, 1944. London, Ian Allan and Pettersson, 2000. Pettersson 1944-09-19 received a letter from general Dwight D. Eisenhower stating “I desire to commend you for your part in the coordination of the operation of the Meteorological Services in support of the 'OVERLORD' assault of the Continent of Europe. Considerable research and long hours of you and your associates resulted in the reconciliation of differences in forecasting methods and the development of a procedure which enabled me to receive the advice necessary for the selection of D-day with confidence that the information received was the best obtainable.” (Nilsen, 2016; 241).
[22] https://www.dagbladet.no/nyheter/norske-meteorologer-avgjorende-for-d-dagen/61395392. Visited: 2018-10-16.
[23] Store norske leksikon. https://snl.no/D-dagen Visited: 2018-10-31.
[24] Dietrichs, ES. 2017. På livets grense [On the border of life]. Oslo, Humanist forlag; 75-ff.
[25] http://www.archive.org/stream/textofconvention00inte#page/n5/mode/2up Visited: 2018-08-30.
[26] Present version is from 1974 and contains many updates. http://www.imo.org/en/About/Conventions/ListOfConventions/Pages/International-Convention-for-the-Safety-of-Life-at-Sea-(SOLAS),-1974.aspx Visited: 2018-08-30.
[27] Engelsen, H. Red. 1926. Legebok for sjømenn [Medical Guide for Seafarers]. Oslo, Norges Røde Kors; ix.
[28] Storsteen, E. Red. 1937. Social håndbok for Norge [Social Handbook for Norway]. Oslo, Norsk Forening for Socialt Arbeide; 798.
[29] International Code of Signals for Visual, Sound, and Radio Communications, United States Edition, 1969.
[30] The Naval Marine Archive. The Canadian Collection. 2012-03-21, http://navalmarinearchive.com/research/history_international_code_signals.html Visited: 2018-10-30
[31] https://www.itu.int/en/history/Pages/DiscoverITUsHistory.aspx Visited: 2019-04-01
[32] Wikipedia: Office International d’Hygiene Publique https://en.wikipedia.org/wiki/Office_International_d%27Hygi%C3%A8ne Publique Visited: 2019-04-01.
[33] Rothblum, AM. 2000. Human Error and Marine Safety. U.S. Coast Guard Research & Development Center. http://www.bowles-langley.com/wp-content/files_mf/humanerrorandmarinesafety26.pdf Visited. 2018-09-17.
[34] Wikipedia: SS Torrey Canyon https://en.wikipedia.org/wiki/SS_Torrey_Canyon Visited: 2018-09-17.
[35] The "Torrey Canyon" Salvage Attempt. http://www.zeesleepvaart.com/torreycanyon.eng.htm Visited: 2018-09-17.
[36] Carpenter, K J. 1986. The History of Scurvy & Vitamin C. Cambridge, Massachusetts, Cambridge University Press; 29.
[37] https://www.uptodate.com Visited: 2018-10-16.
[38] Carpenter, 1986; 3.
[39] Lauring, K. 1999. Skørbug og dens helbredelse - et spørgsmål om teori eller praksis. Helsingør, Handels- og Søfartsmuseets Årbog. 58; 76.
[40] Bown, S. 2003. Scurvy. How a Surgeon, a Mariner and a Gentleman Solved the Greatest Medical Mystery of the Age of Sail. London, Summersdale Publishers; 84.
[41] Robertson, D. 2017. Metropolitan Scurvy in the Shadow of the Cook Voyages. The Journal of Pacific History. 52, 1; 16.
[42] Bown, 2003; 36.
[43] Lauring, 1999; 77.
[44] “Scurvy could not be cured because it could not be understood” (Bown, 2003; 11).
[45] “… water-gruel sweetened with sugar in the morning; fresh mutton-broth often times for dinner; at other times puddings, boiled biscuit with sugar etc. and for supper, barley and raisins, rice and currants, sago and wine, or the like.” Lind, J. 1753. A treatise of the scurvy. Edinburgh; 191.
[46] Lind, 1753; 191.
[47] Carpenter, 1986; 52.
[48] Thelle, Dag S. 1993. Språk i Norden. Om skjørbuk, øl og sitrusfrukter [Language in Scandinavia. On scurvy, beer and citrus]. Oslo, Tidsskrift for den Norske Lægeforening [Journal of the Norwegian Medical Association]. 113; 638.
[49] White, Marcus. 2016-10-04. James Lind. The man who helped to cure scurvy with lemons. BBC News. https://www.bbc.com/news/uk-england-37320399 Visited. 2018-10-31.
[50] https://www.cochrane.org/news/international-clinical-trials-day-2018 Visited: 2018-10-31.
[51] Wikipedia: Limey. https://en.wikipedia.org/wiki/Limey Visited: 2019-04-09.
[52] Norum, KR. Et. al. 2002. Axel Holst og Theordor Frölich - pionerer i bekjempelsen av skjørbuk [Axel Holst and Theodor Frolich--pioneers in the combat of scurvy]. Oslo. Tidsskrift for den Norske Lægeforening [Journal of the Norwegian Medical Association]. 122; 1686-7.
[53] Holst, A. Et. al. 1907. Experimental Studies relating to Ship-beri-beri. I. Introduction. On Polyneuritis of Poultry (polynenritis gallinarum Eijkman) II. On the Etiology of Scurvy. The Joumal of Hygiene. 7; 619-671.
[54] Asdal, K. 2014. Contesting the Animal Model- Axel Holst and the Controversy over Scurvy and Beriberi. Social History of Medicine. 27, 3; 577–593.
[55] Funk, C. 1912. The etiology of the deficiency diseases. Beri-beri, polyneuritis in birds, epidemic dropsy, scurvy, experimental scurvy in animals, infantile scurvy, ship beri-beri, pellagra. Journal of State Medicine. 20; 341–68.
[56] Ranek, MJ. Et. Al. 2011. Albert Szent-Györgyi, MD, PhD. Discoverer of Vitamin C and a Pioneer of Cellular Respiration, Muscle Physiology, and Cancer Development. Labmedicine. 42, 11; 694-698.
[57] Golden, FStC. 1979. Physiological changes in immersion hypothermia, with special reference to factors which may be responsible for death in the early rewarm phase. University of Leeds, PhD.
[58] Anon. 2014-04-03. Obituary Surgeon Rear-Admiral Frank Golden. The Telegraph.
[59] Lind, J. 1762. An essay on the most effective way of preserving the health of seamen in the Royal Navy.
[60] Critchley, M. 1943. Shipwreck Survivors. A Medical Study. London, J. and A. Churchill. Anon. 1943. A Guide to the Preservation of Life at Sea after Shipwreck. Medical Research Council War Memorandum. London, H.M. Stationery Office.
[61] Golden, F. Et al. 1997. Review of rescue and post immersion problems - a medical ergonomic viewpoint. Guildford, Robens Institute, University of Surrey. 41 pp. IMO has also developed a guide for survival in cold water (IMO. 2012. Guide for cold water survival).
[62] Andersen, P. 1913. Bidrag til søartilleriets historie [Input to the history of naval artillery]. København; 8.
[63] Originally called Sea Cadet Company [Søe Cadet Compagniet]. https://en.wikipedia.org/wiki/Royal_Danish_Naval_Academy Visited: 2016-12-30.
[64] Wikipedia; Royal Norwegian Naval Academy https://en.wikipedia.org/wiki/Royal_Norwegian_Naval_Academy Visited: 2018-10-31.
[65] Reglement for et institut til at danne officierer for den norske søetat [Regulations for an institute to educate officers for the Norwegian Navy]. Royal Decree of 1816-12-23.
[66] Mellbye, F. 1964. Utbygging av helsevesenet for sjømenn [Development of a health care system for sailors]. Oslo, Tidsskriftet for den norske Lægeforening [Journal of the Norwegian Medical Association]. 84; 1275-1277.
[67] ILO. 1946. Convention No 73 On Medical Examination (Seafarers) Convention.
[68] The Norwegian Shipping and Trade Mission (NORTRASHIP). https://en.wikipedia.org/wiki/Nortraship Visited: 2019-04-02.
[69] https://www.warsailors.com/oddconrad.html Visited: 2019-04-02.
[70] Hoffmann, WC. 1945. Krigsnevroser i vår handelsflåte under den 2. verdenskrig [War neuroses in our merchant marine during the Second World War]. Oslo, Tidsskrift for den norske Lægeforening [Journal of the Norwegian Medical Association]. 65; 419-421.
[71] Helweg-Larsen, P. Et. al. 1952. Famine Disease in German Concentration Camps. Acta Psychiatr Neurol Scand Suppl. 83; 1-460.
Pop up: October 9th is designated Leif Erikson Day by the American Congress in 1964. The date was selected because it was the date in 1825 when the ship «Restauration» from Stavanger arrived in New York with 52 Norwegian immigrants on board - the first organized emigration from Norway to North America.
Pop up: King Håkon Håkonsson (1217–1263) gave the Bergen merchants a monopoly on trade with Northern Norway, a monopoly that held until 1715. Dry fish made Bergen one of the biggest trading centre at the time.
Pop up: VOC was founded on March 20th 1602 and closed down In 1799. VOC was the first company to issue shares that could be bought by anybody (https://en.wikipedia.org/wiki/Dutch_East_India_Company Visited: 2018-10-15). Many Norwegians took employment on VOC ships VOC (Sogner, S. 1994. Ung i Europa. Norsk ungdom over Nordsjøen til Nederland i tidlig nytid. Oslo, Universitetsforlaget).
Pop up: The territorial limit is today 12 nautical miles. In addition, costal states have 200 miles economic zone. Before 1982 there was a lot of disputes on borders at sea and especially on the issue of fishing rights. One example is the three cod wars between Great Britain and Iceland (1958-1961, 1972-1973 and 1975-1976). (https://en.wikipedia.org/wiki/Cod_War Visited: 2018-10-15).
Pop up: Robert FitzRoy var commanding officer on HMS «Beagle» on which Charles Darwin sailed to South America in 1833.
Pop up: Sverre Petterssen was professor at Massachusetts Institute of Technology (MIT) from 1939-41. He was asked to come to England to support the meteorological institute with weather forecasts for the Royal Air Force. He was lieutenant colonel in the Technical Board of the Norwegian Joint Defence Command [Forsvarets Overkommandos Tekniske Utvalg] 1942-45). His forecasts were important for operations against Tirpitz and operation Shingle in Italy. Before the war he had been in charge of the weather forecasting in Western Norway. Litterature: Petterssen, S. 1974. Kuling fra Nord. En Værvarslers Erindringer. Selvbiografi. Oslo, Aschehoug. American edition: Petterssen, S. 2000. Weathering the Storm. The D-Day Forecast and the Rise of Modern Meteorology. American Meteorological Society.
Pop up: “The first International Code was drafted in 1855 by a Committee set up by the British Board of Trade. It contained 70,000 signals, it used eighteen flags and it was published by the British Board of Trade in 1857 in two parts; the first containing universal and international signals and the second British signals only. The book was adopted by most seafaring nations.” (The Naval Marine Archive. The Canadian Collection. 2012-03-21, http://navalmarinearchive.com/research/history_international_code_signals.html Visited: 2018-10-30). Before the middle of 1800s there was a host of different systems of signalling, but all of these systems were either private or naval.
Pop up: To which extent scurvy was known in ancient times is debated. The problem is that if we look for diagnoses, we pose an unhistorical question. Doctors did not “think” in diagnosis, but in symptoms. The symptoms were not combined into illnesses or diagnosis’. Classification as a scientific tool was an invention of the Swedish doctor Carl von Linnés (1707-1778). As a side it is interesting to note that he also was the surgeon general of the Swedish navy. Dr Thomas Sydenham (1624-1689) extended Linnés large project of classification to medicine.
Pop up: Hoffmann did not find many studies on war neuroses in sailors. The only one he found was a study of 40 sailors having been torpedoed. Margolin, S. Et. Al. 1943. Acute Emotional Disturbances in Torpedoed Seamen of the Merchant Marine, who are continuing at sea. War Medicine. 3; 393-408.
ADAPTED BY TIM CARTER FROM SECOND EDITION BY A J ULVEN AND L HOLDERNESS
The management of risk in the maritime industry has a long history. Risks of concern to the industry are many and varied and include:
Shared ownership of ships and their cargoes was an early form of risk pooling. Insurance markets then developed to cover financial losses associated with maritime risks. Classification systems for assessing a ship’s seaworthiness were developed and used to determine the level of premium required to insure vessel and cargo. Capital spending and crewing policies, while not amenable to cover in the normal insurance market, often have their risks managed by ship chartering or by outsourcing of ship and crew management to specialist contractors.
The systematic management of health, safety and environmental risk has been a relatively late addition to the risk reduction techniques used in the maritime industry. The industry rarely developed active approaches, except in sectors where risks to corporate image mattered, such as passenger transport and tanker fleets owned by oil majors. Thus, most developments have been the result of international agreements such as the IMO conventions on control of pollution and the introduction of risk based approaches in the International Ship Management (ISM) code.
A risk assessment[1] is a structured examination that includes
If measures are already in place the risk assessment will also include an assessment of the effectiveness of these measures. Components of a risk assessment may also include evaluating the likelihood of events happening together. The assessor must make a best estimate of how probable or likely a harm or loss is to occur and an estimate of the worst-case impact or consequence if it does occur, that is, the most severe rational scenario of harm. Risk assessment requires the assessor to ask a lot of ‘what if’ questions and is ideally an objective evaluation of risk based upon reliable data. However, due to a lack of objective data, it is often based on subjective assumptions of potential loss and probability of occurrence. The assessor must consider and assess uncertainties, and the chance of error in the assumption of potential and probability is large.
It is good practice for a risk assessment to be undertaken, and all identified necessary measures implemented, before carrying out a task. All tasks should be risk assessed in a depth that is proportionate to the level of anticipated risk. A risk assessment is a practical exercise and needs to relate to the situation in which the risk occurs. Hence, in order to fully understand the nature of the activity, a visit to the workplace or a representative worksite is often necessary in the course of a risk assessment.
A hazard is something with the intrinsic potential to cause harm. This could be a technology, substance, form of energy, biological agent etc. Wikipedia, the free encyclopedia provides a concise definition: “A hazard is any biological, chemical, mechanical, environmental or physical agent that is reasonably likely to cause harm or damage to humans, other organisms, or the environment in the absence of its control.”[2]
The identification of potential hazards is the first step in performing a risk assessment.
Assess the likelihood and severity of the harm that could be caused to people, ship operations or the environment. What are the potential consequences?
The likelihood of a hazard causing harm should be within the business, within the wider company group or within the industry sector. Data may or may not be available for the incidence of such events.
The severity is the amount of harm or loss that the hazard is able to cause if there is human or environmental exposure to it. In considering the potential for harm and loss, the following factors should be taken into account:
Risk can be defined as the probability or likelihood that exposure to a hazard will lead to a negative consequence. The level of risk is often evaluated considering the equation below.
Risk = Likelihood or probability of the harm or loss occurring x How much harm or loss/severity/consequence
Many organisations and advisers utilise a risk matrix that is based on a scale of likelihood or probability and impact or consequences. Many such matrices are available and the terminology may differ. It is important to be clear on the terminology to be used in each risk assessment as different phrases may mean different things to different people. (Cross reference AMH medical selection). Evaluating the level of risk on such a matrix provides the initial level of risk.
If the level of risk is not acceptable measures to remove the hazard, decrease the likelihood of the hazard causing harm and/or reduce the severity of the harm or consequence must be considered. I control measures are currently in place their effectiveness can be asessed’. If additional control measures are necessary to bring the degree of risk down to a level that is tolerated these must be implemented and assured. The level of risk should be reduced so far as is reasonably practicable. Some methods of control are inherently more reliable than others. The more reliable methods should always be the preferred choice.
Each stage of the risk assessment should be recorded and communicated to all personnel who are involved in the task.
Risk assessment is an ongoing process and must be reviewed regularly. A review should be undertaken immediately if there is reason to believe that the assessment is no longer valid, for instance an injury or a health problem that may be attributable to it, or if there has been a significant change in the work to which the assessment relates.
The ‘precautionary principle’ underlies any ethically sound risk assessment. Its basis is to assume that the worst case can happen, both in terms of uncertain severity and uncertain probabilities. It is important to have in mind the uncertainty of possible harmful effects even if exposure is lower than the level considered to be safe. The precautionary principle is a well-established approach to the assessment of major hazards and depends on a realistic consideration of worst-case scenarios.
A working definition of Precautionary principle is given by the World Commission on the Ethics of Scientific Technology (COMEST):
http://unesdoc.unesco.org/images/0013/001395/139578e.pdf (accessed 2 Jan 2020)
“When human activities may lead to morally unacceptable harm that is scientifically plausible but uncertain, actions shall be taken to avoid or diminish that harm.
Morally unacceptable harm refers to harm to humans or the environment that is:
The judgment of plausibility should be grounded in scientific analysis. Analysis should be ongoing so that chosen actions are subject to review.
Uncertainty may apply to, but need not be limited to, causality or the bounds of the possible harm.
Actions are interventions that are undertaken before harm occurs and that seek to avoid or diminish the harm. Actions should be chosen that are proportional to the seriousness of the potential harm, with consideration of their positive and negative consequences, and with an assessment of the moral implications of both action and inaction. The choice of action should be the result of a participatory process.”
Risk management implies the use of risk assessment to develop and implement effective preventative strategies (see 7.2).
The International Organization for Standardization (ISO) identifies the following principles of risk management.
Risk management should:
A risk with a large potential loss and a low probability of occurring is often treated differently from one with a low potential loss and a high likelihood of occurring. In theory, both are of nearly equal priority, but in practice it can be very difficult to establish priorities when faced with a scarcity of resources, especially time, in which to conduct the risk management process. Also the political and media response to risk will push those involved in taking steps to avoid rare major events, even at the expense of far more common low level ones that account, on average for a larger number of casualties. This can be well seen in the priority given to preventing rare ship disasters, while paying little attention to the far larger toll of individual death and disability from injuries and occupational disease in the maritime workplace.
The hierarchy of control options for safety, health and environmental risk is reviewed in 7.4. 33-37 detail the measures used to manage work related health risks.
Monitoring is the measurement or observation to check that risk management is working as expected.
The objectives of risk monitoring and updating are to:
Evaluation is the process of confirming that the whole risk management system is adequately controlling the anticipated risks.
A risk management plan can never be perfect. Critical evaluation at every stage is of great importance. Especially at an early stage it is necessary to match the outcomes of the risk management plans with its objectives. A thorough investigation of each activity in a risk management plan is required. After evaluating the effectiveness and efficiency of all the activities, it is may be necessary to make changes in the action plan to get the desired results. If the risk management plan produces the desired results, it may not need any changes.
It is necessary to review in order to confirm that any changes to the risk management system that have been implemented have led to reductions in risk.
This may be done by recording the possible outcomes of the changed activity and matching them with the main objectives of the risk management plan and then looking for changes to the frequency and severity of the actual outcomes
Evaluating a risk management plan is sometimes a time consuming process that requires expertise, knowledge and experience.
Clear communication to inform all those who may be at risk is essential, but it is also important to enure that anyone who could either reduce on increase risk to themselves or to others understands the nature and severity of risk. They also need to be personally committed to taking the actions needed to maintian control and prevent harm to themselves, fellow workers or to the integrity of vessel operations. All levels of management have roles to play in supporting this as well as avoiding giving conflicting signals about the relative importance of safety, speed or economy.
Seven cardinal rules for the practice of risk communication have been proposed (U.S. Environmental Protection Agency):
The hierarchy of reliability for control measures is well established, especially in relation to good occupational hygiene practice for the control of chemical (Ch. 6.4) and physical agents (CH. 6.3) that pose a risk to health. However, the same principles apply, with some minor modifications, to the control of injury risks and threats to the wider environment [cross reference needed]. Elimination of the risk or engineering controls are always better than those which rely solely on task management or personal protective equipment.
The following questions need to be answered in sequence when control measures based on the results of a risk assessment are being planned.
This is the most effective option but is only possible where there are viable alternatives. Alternatives may increase capital or operating costs. Examples include:
- asbestos is no longer used in ship construction because of its long term health effects
- the use of marine diesel rather than residual fuel oil for propulsion greatly reduces emissions of sulphur in flue gasses
- ceasing to use caustic soda for tank cleaning reduces the risk of chemical eye injuries.
It is usually far more cost-effective to introduce engineering controls at the design stage for a ship. Retrofitting can be expensive and is not always practicable. Examples include:
- noise exposure in engine spaces has been the cause of deafness in marine engineers. Design to reduce noise levels, engines spaces that can be left unmanned and noise insulation for engine control rooms greatly reduces exposure.
- on board sewage and ballast water treatment systems prevent the release of harmful substances or alien species into the marine environment.
- the use of inert gasses to blanket flammable bulk liquid cargoes, such as hydrocarbons reduces the likelihood of explosions and fires.
- the design of shipping containers to eliminate work at a height when they are stowed reduces the risk of falls.
The consistent use of safe working practices depends on the workforce understanding their rationale and regarding them as practicable, and on active supervision by managers who believe in their importance, even when they can delay task completion. Examples include:
Monitoring and the frequent (re)evaluation of control measures and any changes to them, (7.3) form the basis for assessing the effectiveness of risk control. At one level, it is possible to use the volume and cost of claims to insurers to assess the adequacy of control in financial terms. However, for health, safety and environmental risks this method will underestimate the scale and severity of harm.
The primary measures that can be used are specific indicators, for example, the frequency of death, injury or illness in people and measures of environmental harm such as loss of biodiversity of the seas, coastal areas and the air. However these measures often show a long lag period between the existence of a risk factor and the harm becoming apparent, for example an occupational cancer or noise induced deafness, even when methods are in place to measure relevant indicators. It is also ethically questionable to await such effects if the risk assessment has anticipated their occurrence.
Where the assessment process identifies specific risks it is often possible to use secondary monitoring measures to evaluate the adequacy of control. For instance, levels of noise may be measured to give an early warning of the risk of deafness, thus enabling better noise controls to be introduced. Similarly levels of flue gas emissions may indicate the risks of air pollution – especially in port areas where onshore populations may be harmed. This can indicate the need for measures, such as the use of less polluting fuels or supply of electricity from ashore to allow ship’s generators to be taken off line and reduce emissions.
No risk assessment will be perfect. While it should be based on the best current knowledge there will always be new and unexpected hazards. Alertness is needed to recognise these at the earliest opportunity so that action can be taken across the industry to minimise harm. An example of this was the recognition that deaths were occurring on ships carrying wood pellets, where the cargo was unexpectedly releasing toxic carbon monoxide into enclosed hold areas. Recognition has enabled new controls such as ventilation prior to hold access and the use of gas detectors to bring this new risk under control.
[1] https://www.hse.gov.uk/simple-health-safety/risk/index.htm Accessed January 5 2020